
How Much Does It Cost to Implement Epic? Maximize UAT Value
Picture walking into a restaurant where the menu has no prices. That’s how many healthcare organizations feel when they first consider Epic implementation costs. The sticker shock can be real – but let’s cut through the mystery.
Think of implementing Epic like building a custom home. The foundation might cost the same, but your final price depends on your unique needs, size, and how fancy you want to get with the features. A small clinic won’t need the same setup as a sprawling hospital network.
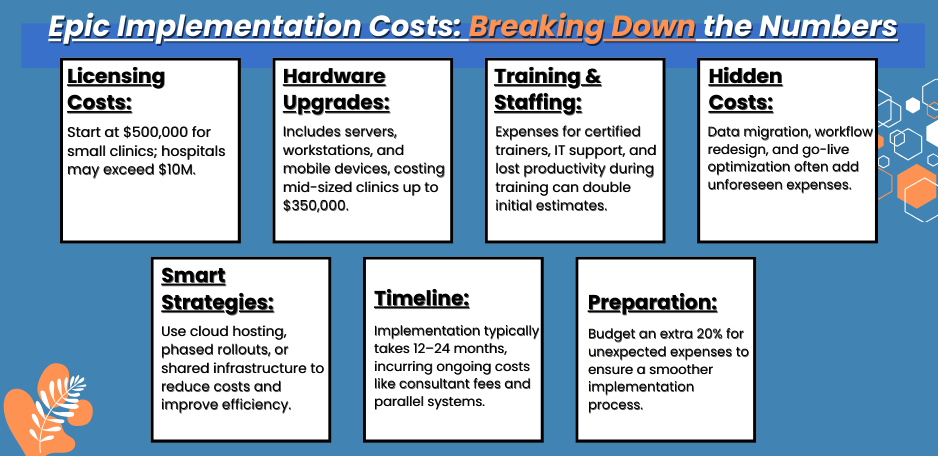
Here’s something surprising – the smallest organizations implementing Epic often spend between $500,000 to $1 million. A jaw-dropping number? Sure. But like buying a Tesla instead of a basic sedan, you’re paying for an ecosystem, not just software.
Speaking of unexpected truths – many clinics focus on the software cost while underestimating the human factor. Beckers Hospital Review revealed that staff training and workflow redesign often eat up 40% of the total cost to implement Epic in smaller settings. Think about that: nearly half your budget goes to getting your team comfortable with their new digital home.
Your Epic journey might remind you of renovating a house while living in it. You’ve got to keep seeing patients, running labs, and managing billing and this adds hidden costs that many forget to factor in.
But here’s where it gets interesting – smaller clinics actually have some advantages. They’re more nimble, can make decisions faster, and often complete implementation in half the time of larger organizations. One family practice in Colorado managed their entire Epic rollout in just four months, coming in under their million-dollar budget.
The Epic implementation landscape keeps evolving. As cloud hosting options are making it more accessible for smaller players, some clinics are finding creative ways to partner with larger health systems to share costs. Others are phasing their implementation to spread the investment over time.
This is where expert guidance becomes gold. Like having a seasoned architect for your dream home, the right implementation partner can spot potential issues before they become expensive problems. They’ve seen the pitfalls, know the shortcuts, and understand how to scale solutions to your size.
Understanding Epic Implementation Costs
Picture a puzzle where every piece affects your bottom line – that’s what the cost to implement Epic EHR looks like. Let’s break this down in a way that actually makes sense.
Remember that fancy coffee machine you bought? The price tag wasn’t just about the machine – you needed the grinder, filters, and someone to teach you all those fancy settings. Epic’s the same way, just with more zeros.
The Core Price Tag
Base licensing hits different depending on your size. Small clinics might look at $500,000 to $1.5 million just for the software. Bigger hospitals? They’re often staring at $5-10 million. But that’s just the opener – like buying a car before adding insurance, gas, and maintenance.
The Hardware Reality Check
Here’s something people don’t talk about enough – your old computers might not cut it. The Epic EMR cost includes beefing up your tech:
– New servers (unless you go cloud)
– Workstation upgrades
– Mobile devices for providers
– Backup systems that actually work
A mid-sized clinic recently shared their hardware bill: $350,000. They thought they’d save money using existing computers. Spoiler alert: They ended up spending more to replace them gradually than if they’d done it all at once.
The People Factor
Nobody mentions this upfront, but the cost to implement Epic is heavily weighted toward people:
– Epic-certified project managers ($175-250k annually)
– Training specialists ($80-120k each)
– Extra IT support during go-live
– Overtime for staff training
One surgery center learned this the hard way. They budgeted for trainers but forgot about covering shifts while people trained. Their actual training costs doubled their initial estimates.
Timeline Truths
Implementation usually takes 12-18 months for smaller setups, and 18-24 for larger ones. During this time, you’re paying for:
– Project team salaries
– Consultant fees
– Lost productivity during training
– Parallel systems running together
The Hidden Costs
Nobody talks about these, but they’re real:
– Workflow redesign consultants
– Custom interface development
– Data migration specialists
– Post-go-live optimization
A family practice in Minnesota got surprised by interface costs alone – $200,000 they hadn’t planned for. Their lab system needed special attention to play nice with Epic.
Smart Money Moves
Some organizations are getting creative:
– Sharing implementation costs with partner hospitals
– Phasing in modules over time
– Using remote training options
– Joining Epic’s community connect program
Remember – these numbers aren’t set in stone. Like a home renovation budget, you’ll want to add 20% for surprises. Because there will be surprises.
The Bottom Line
Small clinic? Plan for $1-3 million all in.
Mid-sized practice? $3-7 million might be your range.
Full hospital? You’re looking at $10 million and up.
But here’s the thing – focusing purely on cost misses the point. It’s like comparing the price of hammers without thinking about what you’re building. The right question isn’t just “How much?” but “What value will we get?”
Smart organizations are thinking long-term. They’re not just buying software; they’re investing in their future workflow, patient satisfaction, and competitive edge.
Licensing Costs
Here’s a truth about how much Epic costs to implement that might surprise you. The licensing fees feel like buying a house – except the price changes based on how many rooms you’ll actually use.
Small clinics often blink twice at the numbers. Basic Epic licensing starts at around $500,000, and that’s before adding specialized modules. One family practice in Arizona thought they’d need just the basics – then realized they needed four extra modules at $75,000 each. Nobody saw that coming.
The cost to implement Epic EHR varies wildly based on what you’re running:
– Primary care needs fewer modules
– Specialty practices require specific tools
– Multi-specialty clinics need the whole enchilada
Let’s talk real money. A recent surgery center shared their breakdown:
Base license: $600,000
Essential modules: $250,000
Patient Portal: $85,000
Mobile access: $45,000
But here’s what makes Epic cost for a small clinic interesting – it’s not just about size. A five-provider specialty practice might need more expensive modules than a ten-provider primary care office. It’s like buying camera gear – a professional photographer might spend more on one lens than an amateur spends on their whole setup.
Epic’s pricing model includes some surprises:
– You’ll pay per provider, not per user
– Some modules are bundled, others aren’t
– Maintenance fees kick in after year one
– Interface costs vary by connection type
One pediatric clinic found a clever workaround. They joined a larger health system’s Community Connect program. Instead of paying full Epic license costs, they essentially “rent” access. Their total came to about 40% of what direct licensing would have cost.
Watch out for these license-related gotchas:
– Growth fees when adding providers
– Extra costs for temporary staff
– Charges for multiple locations
– Special pricing for part-time providers
Think about licensing like a gym membership – basic access gets you in the door, but special classes (modules) cost extra. And just like that membership, you’ll keep paying to keep it active.
Annual maintenance typically runs 15-20% of your initial license cost. One urgent care center budgeted for the first year but forgot about ongoing maintenance. That oversight led to some interesting budget discussions in year two.
Smart organizations are negotiating hard on these fees. Some get creative with volume discounts, while others phase in modules over time. The key? Know what you need before you sign.
Infrastructure Costs:
Let’s talk about the nuts and bolts of cost to implement Epic – the stuff nobody mentions in the sales pitch but hits your wallet just as hard.
Think of infrastructure like the plumbing and wiring in your house. Nobody sees it, but try running things without it. One urgent care learned this when their old network crumbled under Epic’s demands. Their “small” infrastructure upgrade? Turned into a $200,000 project.
Here’s what’s typically on your shopping list:
– Servers that can actually handle the load
– Network upgrades for smooth performance
– Storage systems that keep everything safe
– Backup solutions that work when you need them
The Epic EMR cost for infrastructure breaks down differently than you might expect. A family practice in Texas shared their real numbers:
Network upgrade: $75,000
Server setup: $150,000
Storage solution: $50,000
Backup systems: $25,000
But here’s where it gets interesting – cloud options are changing the game. Some clinics skip the big server room entirely. They’re paying monthly instead of dropping huge upfront cash. One pediatric group saved $100,000 going this route.
Remember when we talked about how much Epic costs for a small clinic? Infrastructure might eat 20-30% of your budget. But smart planning can trim that down:
– Start with a thorough tech assessment
– Consider cloud hosting where it makes sense
– Phase upgrades to spread costs
– Look for redundant systems you can eliminate
Watch out for these hidden infrastructure costs:
– Power system upgrades
– Cooling system improvements
– Security enhancements
– Ongoing maintenance contracts
One clever move? Some smaller practices share infrastructure costs with partner organizations. A group of three independent clinics in Colorado split their server costs, saving each practice about 40%.
Remember – good infrastructure is like good health insurance. It seems expensive until you need it. Then it’s priceless.
The key? Plan for growth. Your infrastructure needs to handle not just today’s load, but next year’s too. Because upgrading twice costs more than doing it right once.
Training and Staffing Costs
Let’s tackle the part of how much it costs to implement Epic that often blindsides healthcare organizations – the people factor.
Think of training as teaching someone to drive. Sure, you could just hand over the keys, but that’s asking for trouble. One community hospital found this out when they cut corners on training. Their mistake cost them an extra $300,000 in post-go-live support.
The real cost to implement Epic EHR for training hits different areas:
– Super-user training (your in-house experts)
– End-user training (everyone else)
– Go-live support (your safety net)
– Ongoing education (keeping skills sharp)
Here’s what shocked a recent specialty practice:
Initial super-user training: $80,000
Staff training program: $150,000
Go-live support: $200,000
Lost productivity: $175,000
Nobody talks about that last one. When your staff’s learning Epic, they’re not seeing patients. That revenue dip? It’s real.
Speaking of real numbers, implementing Epic needs dedicated people:
– Project managers
– Application analysts
– Training coordinators
– Technical support
One smart move came from a primary care group. They trained extra super-users early on. Seemed expensive at first, but when go-live hit, they needed way less outside help.
Watch these hidden training costs:
– Travel for certified training
– Overtime during learning sessions
– Temporary staff coverage
– Refresher courses
Here’s a trick some places use: They schedule training in waves. Instead of shutting down the whole clinic, they keep some providers seeing patients while others learn. Takes longer but hurts less financially.
Think about staffing costs like building a sports team. You need:
– Coaches (trainers)
– Players (end users)
– Support staff (IT team)
– Specialists (consultants)
Most surprising cost? Post-go-live optimization. One clinic thought they were done after training. Six months later, they spent another $100,000 getting workflows right.
Remember: Skimping on training is like buying a Ferrari and never learning to drive a stick. You’ll either crash or never get out of first gear.
Smart organizations budget for the long game. They know good training upfront means fewer headaches (and costs) later. Because in healthcare IT, like in medicine, prevention beats cure every time.
Hidden Costs in Epic Implementation
Let’s expose the sneaky costs of Epic implementation that nobody warns you about – the stuff that jumps out like surprise bills after a hospital stay.
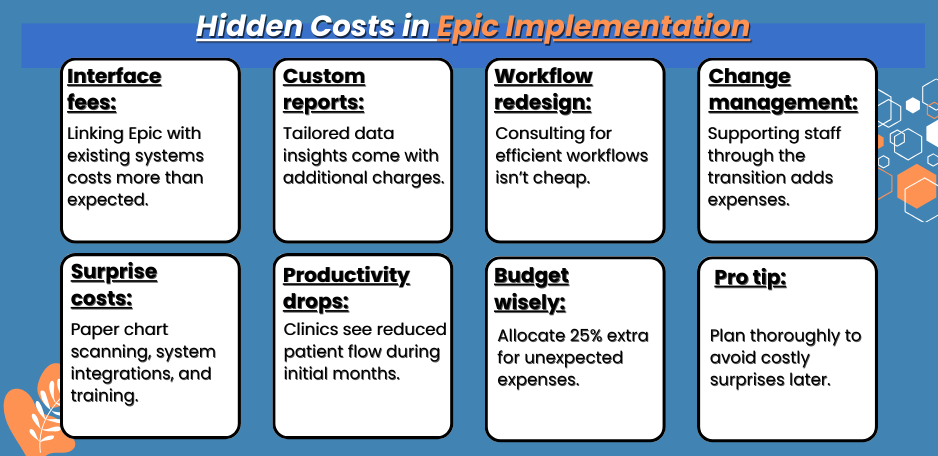
Ever moved to a new house and found costs you never imagined? Epic’s like that, but bigger. One clinic budgeted perfectly for the obvious stuff then got blindsided by $250,000 in “other” expenses. Let’s prevent that from happening to you.
Data migration hits harder than expected. It’s not just moving files – it’s like translating ancient manuscripts. A specialty practice thought they’d spend $50,000 on migration. Reality? $175,000 after cleaning up years of messy records. The cost to implement Epic often doubles here.
Here’s what blindsides most clinics:
– Interface fees with existing systems
– Custom report development
– Workflow redesign consulting
– Change management support
One orthopedic group shared their surprise costs:
Old system maintenance: $45,000
Custom interfaces: $120,000
Workflow consulting: $85,000
Staff overtime: $95,000
Looking at how much Epic EMR costs? Don’t forget these ongoing hits:
– Annual maintenance fees
– Regular upgrades
– Additional training
– System optimization
Here’s a curve ball – productivity drops during the first few months. One primary care clinic saw 30% fewer patients for six weeks. That’s lost revenue nobody plans for.
The real kicker? Epic costs for a small clinic include things like:
– Paper chart scanning
– Third-party tool integration
– Insurance company connections
– Quality reporting setup
Smart clinics are getting creative. One group spread their go-live across departments instead of all at once. Saved them 20% on support costs and kept revenue flowing.
Watch for these budget vampires:
– Emergency IT support
– Last-minute hardware needs
– Extra training sessions
– Temporary staff coverage
Pro tip from a successful implementation: Budget 25% extra for surprises. Sounds high? Every clinic that didn’t wish they had.
Remember: Epic’s like an iceberg – the visible costs are just the tip. The real expenses lurk below the surface, waiting to sink your budget if you’re not ready.
The key? Plan for the unexpected. Because in Epic implementation, like in medicine, it’s not if surprises will come – it’s when.
Maximizing UAT Value
Let’s talk about UAT in Epic – it’s like having a dress rehearsal before opening night, except the tickets cost millions. The cost to implement Epic isn’t just about the software – it’s about making sure it works in real life.
A medium-sized clinic recently shared their UAT story. They thought they could speed through testing to save money. Three months after go-live, they spent $500,000 fixing issues that good testing would have caught for a quarter of that price.
When calculating how much does it cost to implement Epic, here’s what smart testing really costs:
Initial Setup Costs:
– Test environment: $100,000-200,000
– Testing tools: $50,000-75,000
– Training test teams: $40,000-60,000
– Documentation systems: $25,000-35,000
Staff Costs Hit Different:
– Dedicated testers’ time
– Superuser involvement
– Department SME participation
– Leadership oversight hours
One pediatric practice found a clever workaround. They scheduled testing in waves, keeping some providers seeing patients while others tested. Revenue kept flowing, and testing stayed thorough.
The cost to implement Epic EHR during UAT includes hidden players:
– Integration specialists
– Workflow consultants
– Training coordinators
– Technical support teams
Here’s what seasoned implementers know:
– Test real scenarios, not theoretical ones
– Include unusual but critical workflows
– Document everything systematically
– Fix issues as you find them
Watch out for these budget busters:
– Rushed testing cycles
– Incomplete scenario coverage
– Poor documentation practices
– Skipped integration testing
Smart Testing Investments:
– Automated testing tools where possible
– Comprehensive test scripts
– Clear issue tracking systems
– Regular testing checkpoints
One urgent care center’s approach worked brilliantly. They videoed their current workflows before Epic, then tested them against these real-world scenarios. Found 40% more issues than standard testing scripts would have caught.
Real numbers from a recent implementation:
Initial testing phase: $200,000
Integration testing: $150,000
End-to-end testing: $175,000
Performance testing: $125,000
Money-Saving Strategies:
– Use actual staff as testers
– Build reusable test scripts
– Document issues thoroughly
– Test similar functions together
Remember: Good UAT might feel expensive, but bad UAT costs way more. One hospital group learned this when poor pharmacy testing led to a week of manual prescription processing. Cost them triple what thorough testing would have.
The Final Take:
– Budget realistically for testing
– Include all key workflows
– Document everything
– Fix issues immediately
– Train testers properly
Smart organizations know – UAT isn’t where you cut corners. It’s your safety net, your insurance policy, and your peace of mind all rolled into one. Do it right, do it once, and save money in the long run.
Think of UAT like preventive medicine – spend wisely now to avoid costly emergencies later. Because in healthcare IT, like in healthcare itself, prevention beats cure every time.
Best Practices for Cost Optimization
Let’s cut through the noise about how much it costs to implement Epic and focus on what actually saves money without wrecking your implementation.
Think of this like renovating a house – you can cut costs without cutting corners. One community hospital saved $800,000 on their implementation by getting creative with their approach. Here’s the interesting part – they actually ended up with a better system.
Smart Money Moves That Work:
Project Planning Magic
Start with a reality check. A surgical center thought they’d save money by rushing planning. Guess what? They spent twice as much fixing problems that good planning would have caught. The real cost to implement Epic EHR drops when you plan smart.
Their winning formula:
– Detailed workflow analysis before touching Epic
– Staff involvement from day one
– Realistic timeline (not wishful thinking)
– Clear communication channels
Training Tricks That Save Cash
Here’s something cool – a family practice saved $200,000 on training by getting clever:
– Used internal experts as trainers
– Created custom training videos
– Built a peer support network
– Scheduled training in waves
Nobody talks about this, but Epic EMR costs drop significantly when your team actually knows what they’re doing from the start.
Infrastructure Intelligence
One clinic’s smart move? They went cloud-first instead of building a massive server room. Saved $300,000 upfront and cut ongoing costs by 40%. But here’s the catch – you need to know when cloud makes sense and when it doesn’t.
Watch for these money-saving opportunities:
– Virtual servers where possible
– Shared storage solutions
– Phased hardware upgrades
– Smart networking choices
Consultant Collaboration
Here’s a truth bomb – good consultants actually save you money. One medical group tried going solo to save cash. Ended up spending double what consultant fees would have cost fixing preventable mistakes.
Smart consultant use:
– Targeted expertise when needed
– Knowledge transfer focus
– Clear exit strategy
– Measured outcomes
Implementation Intelligence
Think about implementation like building a house – do it right the first time:
– Modular approach to rollout
– Clear success metrics
– Regular progress checks
– Quick issue resolution
One group’s brilliant move? They created a problem-solving team that caught issues early. Saved them $400,000 in post-go-live fixes.
Maintenance Mastery
Future-proof your investment:
– Train internal experts early
– Document everything
– Build strong support networks
– Plan for upgrades
Here’s a secret – maintenance costs drop when your team really owns the system. One practice cut support costs by 50% by investing in deep staff training early.
Workflow Wizardry
Smart workflow design pays off:
– Streamline before automating
– Test thoroughly
– Train effectively
– Monitor constantly
A specialty clinic redesigned their workflows before Epic. Result? They needed fewer customizations, saving $250,000 in implementation costs.
Remember: Cheaper isn’t always less expensive. One hospital “saved” $200,000 on implementation only to spend triple that fixing problems in the first year.
The Bottom Line:
– Plan thoroughly
– Train deeply
– Choose technology wisely
– Use consultants strategically
– Monitor constantly
Smart spending on Epic isn’t about cutting costs – it’s about investing where it matters and saving where it doesn’t. Because in healthcare IT, like in medicine, doing it right the first time is always cheaper than fixing it later.
Unique Insights from Virtelligence
Let’s cut through the sales pitch and talk real numbers about the cost to implement Epic – straight from the trenches, with insights you won’t find in vendor brochures.
Picture this: A clinic in Colorado thought they’d spend $2 million on implementation. After expert guidance, they did it for $1.4 million – and ended up with a better system. How? By knowing where to invest and where to save.
Smart Moves That Actually Work:
– Starting with workflow analysis before writing checks
– Building internal expertise strategically
– Using consultants for complex parts only
– Creating sustainable support systems
When people ask how much does Epic EMR cost, they’re often missing the bigger picture. One pediatric practice saved 30% on their total implementation by following a proven roadmap instead of reinventing the wheel.
Here’s what makes experienced implementation partners worth their salt:
– They’ve seen the pitfalls beforehand
– They know which customizations matter
– They understand where budgets typically break
– They can spot potential issues early
Real talk about Epic costs for a small clinic: Success isn’t about having the biggest budget. It’s about spending smart. Recent projects show:
– Small clinics can implement for $1-3 million
– Mid-sized practices typically need $3-7 million
– ROI usually hits around 18-24 months with proper planning
The Game-Changing Approach:
– Map your current workflows first
– Build realistic timelines
– Train key staff extensively
– Plan for post-go-live support
One family practice found gold in this approach. They thought they needed every Epic module. Expert analysis showed they could start with basics and add later – saved them $400,000 upfront.
Watch These Success Signals:
– Clear project milestones
– Staff engagement levels
– Training completion rates
– Early issue resolution
Remember: Good help pays for itself. A surgical center tried saving money by skipping expert guidance. Six months later, they spent twice what consultation would have cost fixing preventable problems.
The Smart Money Goes To:
– Thorough readiness assessment
– Strategic module selection
– Focused staff training
– Measured rollout plans
Think of it like building a house – you want an experienced architect who’s built similar homes before. They know what works, what doesn’t, and where you can safely save money without compromising quality.
Success isn’t just about going live – it’s about thriving afterward. Smart implementation partners focus on making sure you can run efficiently long after they leave.
The key? Getting it right the first time costs less than fixing it later. Because in healthcare IT, like in medicine, prevention beats cure every time.
Small Clinics vs Large Hospitals
Let’s break down how Epic costs to implement really looks like across different-sized organizations. No sugar coating – just real numbers and experiences.
Small Clinic Reality Check
Think of your neighborhood family practice versus a city hospital. One recent small clinic implementation came in at $1.2 million – way less than they feared after hearing hospital horror stories. They got creative with their approach:
– Shared training resources with other clinics
– Used cloud hosting instead of servers
– Focused on essential modules only
– Built internal expertise gradually
The Big Hospital Scene
When people ask about Epic EMR costs, they’re often shocked by hospital numbers. One 300-bed hospital spent $15 million on their implementation. But here’s the kicker – they generate that much additional revenue every year now because of better billing capture.
Size Matters in Surprising Ways:
Small Clinics:
– More flexible workflows
– Faster training cycles
– Simpler interface needs
– Quicker decisions
Large Hospitals:
– Complex integrations
– Extended training needs
– Multiple department coordination
– Longer implementation times
Here’s what nobody tells you about how much Epic costs for a small clinic – you’ve got advantages:
– Less legacy system baggage
– Fewer workflows to redesign
– More nimble staff training
– Simpler approval processes
A Smart Size-Based Strategy:
Small Clinics (Under 10 providers):
– Basic module package
– Cloud-based solutions
– Phased implementation
– Shared support resources
Large Hospitals:
– Comprehensive module suite
– On-premise infrastructure
– Full-scale project teams
– Dedicated support staff
One clever small practice joined a hospital’s Community Connect program – got Epic for 40% less than going direct. Meanwhile, a large hospital created internal training teams, saving millions over consultant-led training.
Remember: Your size affects your costs, but smart planning matters more than scale. Because in healthcare IT, like in medicine, the right treatment matters more than the size of the hospital.
Final Thoughts
Let’s wrap this up with some straight talk about how much Epic costs to implement – because knowing what you’re getting into makes all the difference.
Think of Epic like building a custom house. The final cost depends on what you need, how you build it, and who helps you along the way. We’ve seen organizations crush their implementations while others struggled, and the difference usually comes down to planning and expertise.
The numbers vary, but here’s what we’ve learned matters most:
– Small clinics can succeed with $1-3 million
– Mid-sized practices typically need $3-7 million
– Large hospitals often invest $10 million plus
But here’s what really determines your Epic EMR costs:
– How well you plan before you start
– Who guides your implementation
– How you train your team
– Which approach fits your size
Remember when we talked about how much Epic costs for a small clinic? Those success stories came from organizations that got expert help early. They knew when to invest and where to save.
Ready to make your Epic implementation a success story? Let’s talk about your specific needs. We’ve guided organizations of every size through successful implementations, and we’d love to help you:
– Plan your budget realistically
– Avoid costly pitfalls
– Choose the right approach
– Maximize your investment
Don’t let uncertainty hold you back. Whether you’re just starting to explore Epic or ready to begin implementation, reach out for a conversation about your unique needs. Because getting Epic right the first time isn’t just about saving money – it’s about transforming your practice for the better.
Contact us today to start planning your successful Epic implementation. Your future workflow will thank you.
FAQs
Let’s answer the real questions people ask about how much Epic costs to implement – no jargon, just honest answers.
What’s the minimum budget we need?
Small clinics should plan for at least $1 million. That’s your starting point for basic modules, training, and infrastructure. One family practice thought they could do it for less – ended up needing $1.2 million for a solid implementation.
Does Epic charge per user or provider?
Epic charges per provider, not per user. Here’s the twist – mid-levels and part-time providers often count differently. A specialty clinic saved $100,000 by understanding these nuances before signing.
How long until we see a return on investment?
Most practices see ROI in 18-24 months. But here’s what affects your timeline:
– How well you train staff
– Which modules you implement
– How quickly you optimize workflows
– Your billing capture improvement
What about ongoing Epic EMR costs?
Plan for annual maintenance fees around 15-20% of your license cost. One urgent care forgot to budget for this – created some interesting conversations in year two.
Can small clinics really afford Epic?
Yes, especially with newer options like Community Connect. Epic costs for a small clinic can be managed through:
– Phased implementations
– Shared resources
– Cloud hosting
– Strategic module selection
What’s the biggest hidden cost?
Staff training and lost productivity during implementation. A medical group budgeted for training but forgot about reduced patient volumes during go-live. That oversight cost them $200,000 in lost revenue.
Do we need consultants?
Most successful implementations use expert help strategically. One practice tried going solo to save money – spent twice as much fixing problems good consultants would have prevented.
Remember: These numbers vary based on your needs and situation. The key is planning smartly and knowing where to invest for the best return.






