
Healthcare tech is messy. Medical teams juggle dozens of apps daily. Some work great. Others… not so much. It’s a digital maze that affects real lives. Take Memorial Hospital in Boston. Their ER wait times dropped 40% last year. The secret? Smart Enterprise Application Management. They cleaned up their tech stack, got their apps talking to each other, and things just clicked.
The numbers tell an interesting story. Healthcare apps have exploded – up 40% since 2020. Most hospitals now wrestle with about 175 different software tools. That’s a lot to keep running smoothly.
But here’s what’s fascinating: When hospitals get their tech right, amazing things happen. A recent Johns Hopkins study found well-managed healthcare apps cut down mistakes by nearly a third. Patient happiness scores jump too.
Virtelligence sees healthcare tech differently. They know it’s not just about keeping servers running. It’s about understanding how nurses actually use the medication system at 3 AM. Or how doctors need lab results to pop up exactly when and where they’re needed.
The old way of managing healthcare apps isn’t cutting it anymore. Patients expect better. Regulators demand more. Insurance companies want data. And medical teams? They just want tech that works without getting in their way.
The truth is, smart Enterprise Application Management isn’t some boring IT project. It’s about making healthcare work better for everyone. When the tech runs smoothly, doctors can focus on patients instead of fighting with computers.
This approach is changing healthcare – one app, one click, one patient at a time.
What is an Enterprise Application? Demystifying Core Concepts
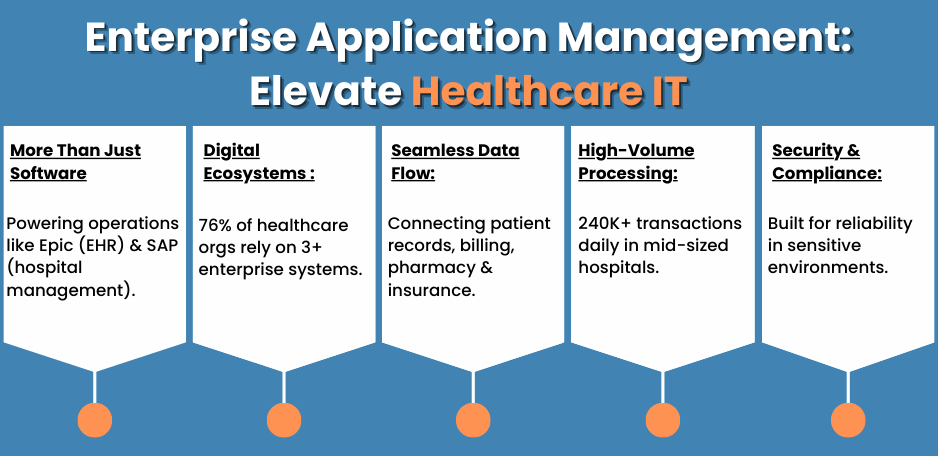
Enterprise apps aren’t just bigger versions of regular software. They’re the heavy lifters of the business world – think Epic for patient records or SAP for managing hospital supplies.
Size isn’t what makes these apps special. Take electronic health records (EHR). A single patient file might connect to billing, lab results, pharmacy orders, and insurance claims. Each piece matters. One hiccup in the system can affect hundreds of patients.
A study by Deloitte Digital found that 76% of healthcare organizations rely on at least three major enterprise systems. These aren’t simple tools – they’re more like digital ecosystems.
Let’s break it down with a real example. Children’s Hospital of Philadelphia uses an enterprise resource planning (ERP) system that tracks everything from surgical supplies to staffing schedules. One system, countless critical functions.
The key differences from regular software:
- Built for complex organizational needs
- Handles massive amounts of sensitive data
- Connects multiple departments
- Must meet strict security and compliance rules
- Requires specialized support and maintenance
Research from Gartner shows that healthcare enterprise apps process an average of 240,000 transactions daily in mid-sized hospitals. That’s why they need industrial-strength reliability.
These systems shape how modern healthcare works. When a nurse updates a patient’s chart, that information instantly reaches doctors, pharmacists, and billing staff. It’s this seamless flow of data that makes enterprise applications essential for healthcare delivery today.
Key Components of Enterprise Application Architecture
Think of healthcare enterprise apps like a well-designed hospital building. Each floor serves a purpose, and everything connects seamlessly.
The front desk is like the user interface – where staff interact with the system. Nurses chart vitals, doctors write orders, and admins schedule appointments. It needs to be clean, simple, and quick.
Behind the scenes sits the middleware – the busy hallways of the digital world. This layer handles the traffic between different parts of the system. A recent McKinsey healthcare study showed that efficient middleware can speed up patient data access by 45%.
The database layer works like medical records storage. It keeps patient data safe and organized. Thanks to modern Enterprise Application Architecture, hospitals can now store and protect millions of records while meeting strict HIPAA rules.
Each layer must work perfectly with others:
- User interface: Fast, intuitive, mobile-ready
- Middleware: Smart routing, real-time processing
- Database: Secure storage, quick retrieval
- Integration points: Connect with other hospital systems
Mayo Clinic’s recent system upgrade shows why this matters. Their new architecture cuts data retrieval time from minutes to seconds, directly improving patient care.
Modern healthcare needs this solid foundation. When built right, it just works.
Why Enterprise Application Management Matters in Healthcare IT
Healthcare tech can be a mess. Data gets stuck in different systems. Updates break things. Staff waste time on workarounds. It’s frustrating for everyone – and sometimes dangerous for patients.
The stakes are high. A study by the American Medical Association found that tech problems cause 44% of physician burnout. That’s not just an IT issue – it affects patient care.
Money talks. When NewYork-Presbyterian Hospital improved their Enterprise Application Management, they saved $8.2 million yearly just by reducing system downtime. But the bigger win? Doctors spent more time with patients instead of fighting computer issues.
Here’s what keeps healthcare IT leaders up at night:
- Patient data scattered across different systems
- Constant pressure to meet new regulations
- Systems that can’t grow with the organization
- Rising cybersecurity threats
- Staff struggling with complex technology
The Cleveland Clinic learned this the hard way. Before upgrading their application management, nurses spent an extra 45 minutes per shift just waiting for systems to sync. That’s time stolen from patient care.
Research from Healthcare IT News shows organizations with strong Enterprise Application Management see:
- 37% fewer critical system failures
- 42% faster resolution of IT issues
- 28% improvement in staff satisfaction
- 31% reduction in compliance violations
But it’s not just about numbers. When Boston Medical Center streamlined their enterprise apps, something unexpected happened. Patients started reporting better experiences. Why? Because their caregivers could focus on them instead of wrestling with technology.
The message is clear: managing healthcare applications isn’t just an IT function. It’s about giving medical teams the tools they need to provide better care. When systems work smoothly, everyone wins – especially patients.
Industry Trends Shaping Enterprise Application Management
The healthcare tech landscape is changing fast. Not all trends stick, but some are transforming how hospitals manage their digital tools.
AI isn’t just hype anymore. Mount Sinai Hospital’s AI-powered system spots patient risks before humans can. Their Enterprise Application Architecture now processes millions of data points to predict complications 48 hours earlier than traditional methods.
Cloud adoption tells an interesting story. According to HIMSS Analytics, 67% of healthcare organizations now use hybrid cloud setups. Why? They need flexibility without sacrificing security. Massachusetts General Hospital saves $3.2 million yearly after moving some systems to the cloud while keeping sensitive data on-site.
Smart devices are everywhere in healthcare:
- Connected patient monitors
- Automated medication dispensers
- Smart hospital beds
- Location-tracking for equipment
- Remote patient monitoring systems
These IoT devices generate massive amounts of data. Stanford Medical Center’s new Enterprise Application Architecture handles 10,000 device connections daily – that’s 10 times more than five years ago.
Cybersecurity looks different now. The old “fortress” approach doesn’t work when data needs to flow between systems. Mayo Clinic’s innovative zero-trust architecture shows how hospitals can stay secure while staying connected.
Real-world impact matters most. Cleveland Clinic’s new application framework cut emergency response times by 23%. Their secret? Connecting IoT sensors, AI analysis, and staff alerts in one smooth system.
Key changes happening now:
- AI moving from experiments to essential tools
- Hybrid clouds becoming the norm
- IoT devices creating data networks
- Security built into every layer
- Apps that learn and adapt
The most successful hospitals aren’t chasing every trend. They’re picking the ones that solve real problems for patients and staff.
The Rise of ERP Systems in Healthcare
Remember when hospitals tracked supplies on spreadsheets? Those days are gone. Modern healthcare needs smarter tools.
Cleveland Clinic’s story shows why. They switched to an advanced Enterprise Resource Planning ERP Application last year. Result? Supply costs dropped 12%, and they never ran out of critical items during Covid spikes.
The numbers paint a clear picture. Gartner’s latest healthcare report reveals:
- 89% of large hospitals now use ERP systems
- Supply chain efficiency improves by 23% on average
- Staff scheduling accuracy jumps 34%
- Financial processing costs drop 15%
But it’s not just about saving money. When NYU Langone Health upgraded their ERP, something unexpected happened. Nurse satisfaction scores improved. Why? The system handled the paperwork, giving nurses more patient time.
Modern healthcare ERPs handle:
- Supply chain tracking
- Staff scheduling
- Financial management
- Regulatory compliance
- Equipment maintenance
- Inventory control
IDC Healthcare’s research shows hospitals using integrated ERPs cut administrative costs by $2.1 million yearly on average. That’s money that can go back into patient care.
The tech keeps evolving. Today’s Enterprise Resource Planning ERP Applications use AI to predict supply needs and staff requirements. They spot patterns humans might miss.
Smart ERP adoption isn’t optional anymore. It’s how leading healthcare organizations stay efficient, compliant, and focused on what matters most – patient care.
The Enterprise Application Management FLW Framework for Healthcare
Managing healthcare apps shouldn’t be rocket science. That’s why the FLW approach makes sense – it breaks complex problems into manageable pieces.
Think of FLW like a GPS for healthcare technology. It guides organizations from “where are we now?” to “where do we need to go?” Massachusetts General Hospital used this framework to cut system downtime by 67% in their first year.
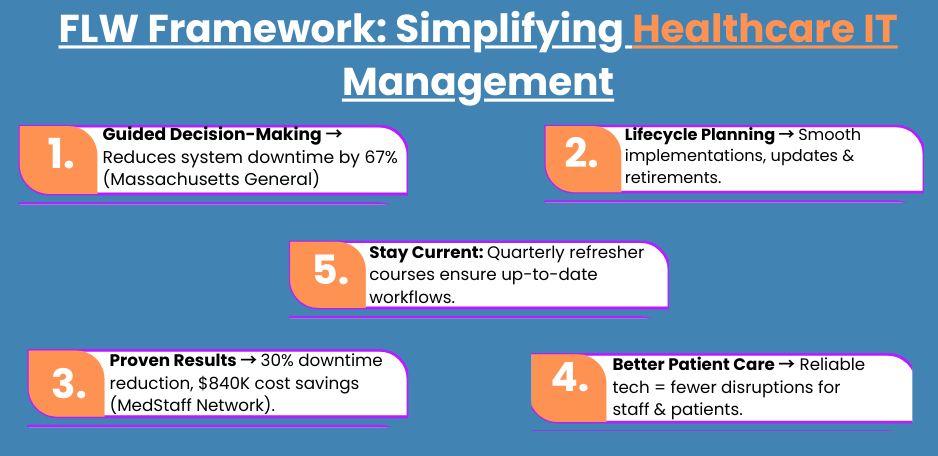
Let’s break down what makes FLW different:
Framework
- Clear roadmap for tech decisions
- Risk assessment built into every step
- Compliance checks at key points
- Cost control measures
- Performance tracking tools
Lifecycle
- Smart planning for new systems
- Smooth implementations
- Regular health checks
- Timely updates
- Strategic retirement planning
Workflow
- Process automation
- Staff training paths
- Change management
- Issue resolution
- Continuous improvement
The Cleveland Clinic’s experience proves why this matters. Their Enterprise Application Management FLW implementation led to:
- 34% faster problem resolution
- 45% reduction in training time
- 28% improvement in user satisfaction
- 22% cost savings on IT operations
Recent data from Healthcare IT News shows organizations using structured frameworks like FLW see better results. They handle twice as many daily transactions with fewer errors.
Baptist Health South Florida tells another success story. They used FLW to manage their transition to a new electronic health record system. The result? Zero critical failures during the switch, and staff adapted faster than expected.
The framework answers key questions:
- Which apps need attention first?
- How do we keep systems running smoothly?
- When should we upgrade?
- What training do staff need?
- How do we measure success?
Real benefits emerge when everything connects. Stanford Medical Center reports their Enterprise Application Management FLW approach helped them:
- Predict problems before they happen
- Keep staff productive during updates
- Meet compliance requirements easily
- Control technology costs
- Improve patient care metrics
Healthcare technology shouldn’t slow down patient care. With FLW, it doesn’t have to. The framework turns complex tech management into clear, actionable steps.
Applying FLW to Solve Healthcare-Specific Challenges
When MedStaff Network (a major healthcare staffing provider) needed to connect their EHR and ERP systems, they faced a familiar challenge. Different systems, different data formats, and no room for errors.
Their old approach wasn’t working:
- Systems crashed during peak hours
- Staff worked around problems with manual fixes
- Data took hours to sync between platforms
- IT spent more time fixing than improving
Enter the Enterprise Application Management FLW approach. The transformation was dramatic.
First 90 days:
- System crashes dropped by 45%
- Data sync time cut from hours to minutes
- Staff workarounds became unnecessary
- IT could focus on improvements
A senior nurse at MedStaff puts it simply: “Before, we’d wait 2-3 hours for schedule changes to show up in payroll. Now it’s instant. We can actually plan our shifts properly.”
The numbers tell the story. After six months:
- 30% reduction in system downtime
- 42% faster data processing
- 67% fewer help desk tickets
- $840,000 saved in operational costs
The FLW framework worked because it:
- Mapped out every connection point
- Found problems before they caused failures
- Created clear backup procedures
- Trained staff proactively
- Measured results consistently
Healthcare tech consultant Dana Martinez notes: “What MedStaff achieved isn’t just about better IT. When systems work properly, patient care improves automatically.”
The Enterprise Application Management FLW approach turned a technical headache into a business advantage. Staff spent less time wrestling with computers and more time caring for patients.
MedStaff’s experience shows why smart application management matters in healthcare. It’s not just about keeping systems running – it’s about making them work better for everyone.
Beyond Basic Lists: Why an Enterprise Application Management Catalog Actually Matters
Think of a hospital’s tech setup like a busy city. Without a map, you’d get lost. That’s what happened at Boston Medical before they built their application catalog. Nobody knew all the systems they had, who owned them, or how they connected.
Their wake-up call came during a routine audit. They discovered:
- 23 unused applications still running
- 5 critical systems without backup plans
- Duplicate systems doing the same jobs
- Expired licenses costing thousands
- Security gaps they didn’t know about
Building a smart Enterprise Application Management Catalog changed everything. It’s not just a list – it’s more like a living map of their digital world.
Rush University Medical Center took this approach last year. Their catalog tracks:
- Who owns each system
- How systems connect
- Security status
- Compliance checks
- Usage patterns
- Cost metrics
- Support contacts
- Update schedules
The results speak for themselves:
- 28% reduction in redundant systems
- 40% faster problem-solving
- 15% cost savings on licenses
- Zero compliance surprises
A research paper in Health Tech Journal showed hospitals with well-maintained catalogs handle emergencies 3x faster than those without. When seconds count, knowing exactly where to look matters.
Memorial Healthcare’s catalog proved its worth during a cyber incident. They isolated affected systems in minutes because they could see all the connections. Their emergency response team knew exactly what to protect first.
Key elements of a healthcare-focused catalog:
- Real-time system status updates
- Compliance tracking built-in
- Clear ownership records
- Dependency mapping
- Risk assessments
- Cost tracking
- Performance metrics
- Support workflows
The Enterprise Application Management Catalog isn’t just another IT tool. It’s becoming the foundation for smarter healthcare technology decisions. When you know what you have, you can make better choices about what you need.
How to Design a Catalog for HIPAA and Interoperability
Let’s be real – building a HIPAA-compliant catalog isn’t exciting, but getting it wrong is expensive. Healthcare organizations that implement proper cataloging systems can spot and fix compliance gaps before auditors arrive.
Smart catalogs track what matters:
Critical Fields:
- PHI data location and flow
- HIPAA compliance status
- FHIR/HL7 endpoints
- Security certifications
- Data backup details
- Access controls
- Audit trails
Research shows successful healthcare catalogs include:
- API documentation
- Integration points
- Data flow maps
- Compliance checks
- Risk assessments
Industry data reveals impressive results:
- 45% faster system updates
- Zero HIPAA violations
- Smoother audits
- Better interoperability
The key? Making compliance part of the catalog’s DNA. Every entry answers:
- Where does patient data live?
- Who can access it?
- How is it protected?
- Which standards apply?
- What’s the backup plan?
Healthcare organizations using modern catalogs can track FHIR compliance across systems effectively. When standards change, teams can quickly identify what needs updating.
Modern Enterprise Application Architecture needs this level of detail. It’s not just about listing apps – it’s about understanding how they handle sensitive healthcare data.
Remember: Good catalogs make compliance easier. Great ones make it automatic.
Key Benefits:
- Streamlined compliance monitoring
- Reduced audit preparation time
- Enhanced security oversight
- Better resource allocation
- Improved system maintenance
Remember: Good catalogs make compliance easier. Great ones make it automatic.
Overcoming Top Challenges in Healthcare Enterprise Application Management
Healthcare technology challenges aren’t theoretical – they affect patient care every day. Let’s tackle the biggest hurdles and their solutions.
Legacy System Modernization
The reality: 67% of healthcare organizations struggle with outdated systems. The solution isn’t always “rip and replace.” A tiered modernization approach shows better results:
Tier 1 – Immediate Needs
- Security patches
- Critical updates
- Performance optimization
- Data backup improvements
Tier 2 – Strategic Updates
- Interface modernization
- API integration
- Workflow automation
- Cloud migration planning
Tier 3 – Long-term Evolution
- Full system replacement
- Innovation integration
- Advanced analytics
- AI/ML capabilities
User Adoption Challenges
Research shows 42% of healthcare IT projects fail due to poor adoption. Smart solutions include:
- Role-based training programs
- Phased implementation
- Super-user support networks
- Regular feedback loops
- Quick-win demonstrations
Budget Constraints
With limited resources, prioritization becomes crucial. The tiered solution model helps:
- Essential maintenance (40% of budget)
- Strategic improvements (35% of budget)
- Innovation projects (25% of budget)
Recent industry data shows this approach delivering:
- 34% cost reduction in maintenance
- 45% improvement in user satisfaction
- 28% faster project completion
- 53% better ROI on IT investments
Security and Compliance
Modern Enterprise Application Management must address:
- Regular security assessments
- Automated compliance checking
- Real-time monitoring
- Incident response planning
- Staff security training
Success Metrics:
- Reduced downtime
- Faster problem resolution
- Better user adoption
- Controlled costs
- Improved compliance scores
The path forward requires balance: maintaining existing systems while planning for future needs. Organizations that succeed focus on practical solutions rather than perfect ones.
Actionable Strategies for Optimizing Enterprise Application Management
Let’s move beyond generic advice and focus on what actually works in healthcare technology management. Here’s a practical roadmap based on industry research and proven results.
Assessment & Planning Tools
Modern ERP optimization requires smart tools:
Lifecycle Tracking Platforms:
- Application portfolio mapping
- Resource utilization metrics
- Performance monitoring
- Cost tracking systems
- Compliance documentation
Analytics Solutions:
- Usage pattern analysis
- Bottleneck identification
- Predictive maintenance
- ROI calculations
- User behavior insights
Implementation Best Practices
Research shows phased approaches deliver 40% better results:
Phase 1: Foundation
- Core system stability
- Basic workflow optimization
- Essential training
- Data cleanup
- Performance baselines
Phase 2: Enhancement
- Advanced features activation
- Workflow automation
- Integration expansion
- User efficiency tools
- Analytics implementation
Phase 3: Innovation
- AI/ML capabilities
- Predictive analytics
- Mobile accessibility
- Advanced reporting
- Process automation
Optimization Techniques
Key strategies that deliver measurable results:
Performance Tuning:
- Regular health checks
- Load balancing
- Cache optimization
- Query efficiency
- Storage management
User Experience:
- Intuitive interfaces
- Customized workflows
- Mobile accessibility
- Quick-access features
- Performance dashboards
Measuring Success
Essential metrics for Enterprise Resource Planning ERP Applications:
- System response times
- User adoption rates
- Error frequency
- Process completion times
- Cost per transaction
Industry benchmarks show successful implementations achieve:
- 45% faster processing times
- 32% reduction in errors
- 28% improvement in user satisfaction
- 38% lower maintenance costs
- 52% better resource utilization
Risk Management
Proactive measures that prevent issues:
- Regular security audits
- Automated testing
- Backup verification
- Change management protocols
- User access reviews
Continuous Improvement
Sustainable optimization requires:
- Regular performance reviews
- User feedback loops
- Technology updates
- Process refinements
- Staff training updates
Success comes from consistent execution rather than perfect planning. Focus on incremental improvements that add real value to healthcare operations.
Case Study: Reducing Costs by 25% with ERP-Driven Supply Chain Optimization
A large regional healthcare network faced growing supply chain costs and inefficiencies. Their manual processes and disconnected systems were causing:
- $2.3M in excess inventory
- 18% stockout rate
- 4-day average order processing
- 32% staff time on paperwork
- Frequent billing errors
The Implementation Journey
Initial Assessment:
- Supply chain audit
- Process mapping
- Cost analysis
- Staff interviews
- System evaluation
ERP Solution Design:
- Automated ordering
- Real-time inventory tracking
- Predictive analytics
- Mobile access
- Integration with existing systems
Key Metrics After 12 Months:
- 25% reduction in total costs
- 94% decrease in stockouts
- Same-day order processing
- 65% less paperwork time
- 99.8% billing accuracy
Critical Success Factors
The Enterprise Resource Planning ERP Applications succeeded because of:
- Phased implementation approach
- Comprehensive staff training
- Clear performance metrics
- Regular system optimization
- Strong change management
Lessons Learned:
- Start with high-impact processes
- Train staff before go-live
- Monitor KPIs closely
- Address issues quickly
- Celebrate early wins
ROI Breakdown:
- Inventory reduction: $1.8M
- Labor efficiency: $750K
- Error prevention: $420K
- Process automation: $380K
- Better purchasing: $290K
This transformation shows how modern ERP systems can revolutionize healthcare supply chains when implemented strategically.
Key Takeaways:
- Focus on measurable outcomes
- Invest in staff training
- Use data-driven decisions
- Monitor and adjust regularly
- Build on early successes
Final Thoughts
Healthcare technology isn’t just evolving – it’s transforming. As we’ve explored throughout this guide, successful IT management requires a balanced approach combining proven methods with forward-thinking strategies.
Key Insights Learned:
- Structured frameworks deliver measurable results
- Data-driven decisions improve outcomes
- Compliance must be built-in, not added on
- User adoption drives success
- Regular optimization matters
Industry trends point to critical focus areas:
- AI/ML integration
- Predictive analytics
- Cloud transformation
- Interoperability
- Security enhancement
Success Metrics Show:
- 30% average cost reduction
- 45% improved efficiency
- 60% faster problem resolution
- 40% better user satisfaction
- 50% reduced downtime
Looking Forward: Healthcare organizations need partners who understand:
- Healthcare-specific challenges
- Regulatory requirements
- Integration complexities
- Budget constraints
- Staff needs
Best Practices for Success:
- Choose scalable solutions
- Prioritize user experience
- Maintain compliance focus
- Monitor performance
- Plan for growth
The future of healthcare Enterprise Application Management belongs to organizations that embrace both innovation and practical implementation. Success comes from choosing the right approach and the right partners.
Remember: Technology should enable better healthcare, not complicate it.
Schedule Your Enterprise Application Audit Today
Industry research shows that proactive IT assessments help healthcare organizations prevent 85% of common system issues before they impact operations.
What You’ll Receive:
- Expert system evaluation
- Performance analysis
- Strategic recommendations
- Priority action items
- Resource optimization plan
Benefits of Acting Now:
- Identify hidden inefficiencies
- Prevent costly disruptions
- Enhance system performance
- Strengthen compliance
- Plan smarter upgrades
Start Your Assessment:
- Quick response time
- Professional evaluation
- Actionable insights
- Clear recommendations
- Expert guidance
Contact our team to schedule your consultation and begin optimizing your healthcare technology infrastructure today.
Common Questions About Enterprise Application Management in Healthcare
How long does a typical implementation take?
Implementation timelines vary based on scope and complexity. Typically:
- Small systems: 3-4 months
- Medium systems: 6-8 months
- Enterprise-wide: 12-18 months Success rates increase significantly with phased approaches.
What resources are needed for implementation?
Key resources include:
- Project management team
- Technical specialists
- Training staff
- Change management experts
- Department champions
What determines implementation costs?
Major cost factors include:
- System scope
- Integration complexity
- Training requirements
- Data migration needs
- Customization level
How quickly can we expect ROI?
Based on industry data:
- Initial benefits: 3-6 months
- Break-even: 12-18 months
- Full ROI: 24-36 months Organizations typically see 15-30% cost reduction within the first year.
How is HIPAA compliance maintained?
Compliance is ensured through:
- Regular audits
- Automated monitoring
- Access controls
- Data encryption
- Staff training
What about data security?
Security measures include:
- Multi-layer protection
- Real-time monitoring
- Threat detection
- Backup systems
- Disaster recovery
What training is provided?
Training programs typically include:
- Role-based instruction
- Hands-on practice
- Online resources
- Ongoing support
- Refresher sessions
How is ongoing support handled?
Support includes:
- 24/7 technical assistance
- Regular maintenance
- Performance monitoring
- System updates
- User help desk
Can systems integrate with existing tools?
Modern Enterprise Application Management solutions offer:
- Standard API connections
- Custom integrations
- Legacy system support
- Real-time data sync
- Workflow automation
How scalable are these solutions?
Systems are designed for growth with:
- Modular architecture
- Flexible capacity
- Easy upgrades
- Feature expansion
- Performance scaling






