
The landscape of healthcare technology transformation reveals fascinating patterns when observed through the lens of experienced implementation specialists. What emerges is a nuanced understanding that successful EHR rollouts hinge on factors that many healthcare executives might find surprisingly human-centric.
Consider how the most successful implementations often unfold: They’re rarely about technical prowess alone. Rather, they reflect a deeper understanding of organizational psychology and clinical workflows The stakes in this arena are extraordinarily high – failed implementations frequently cascade into critical safety concerns, leadership exits, and devastating effects on staff morale.
What’s particularly fascinating is how successful organizations approach these transitions. The secret often lies in what might be called the “cognitive safety net” – a comprehensive support structure addressing both technical and human factors. Organizations that truly excel during these transitions aren’t necessarily those with the most resources, but those who understand the delicate interplay between technology and human adaptation.
Breaking Traditional Patterns
Recent patterns reveal an unexpected correlation: implementations that prioritize staff satisfaction as a key performance indicator tend to achieve smoother transitions. This might seem counterintuitive in what appears to be a purely technical rollout, yet it consistently emerges as a reliable predictor of success.
The Architecture of Smooth Transitions
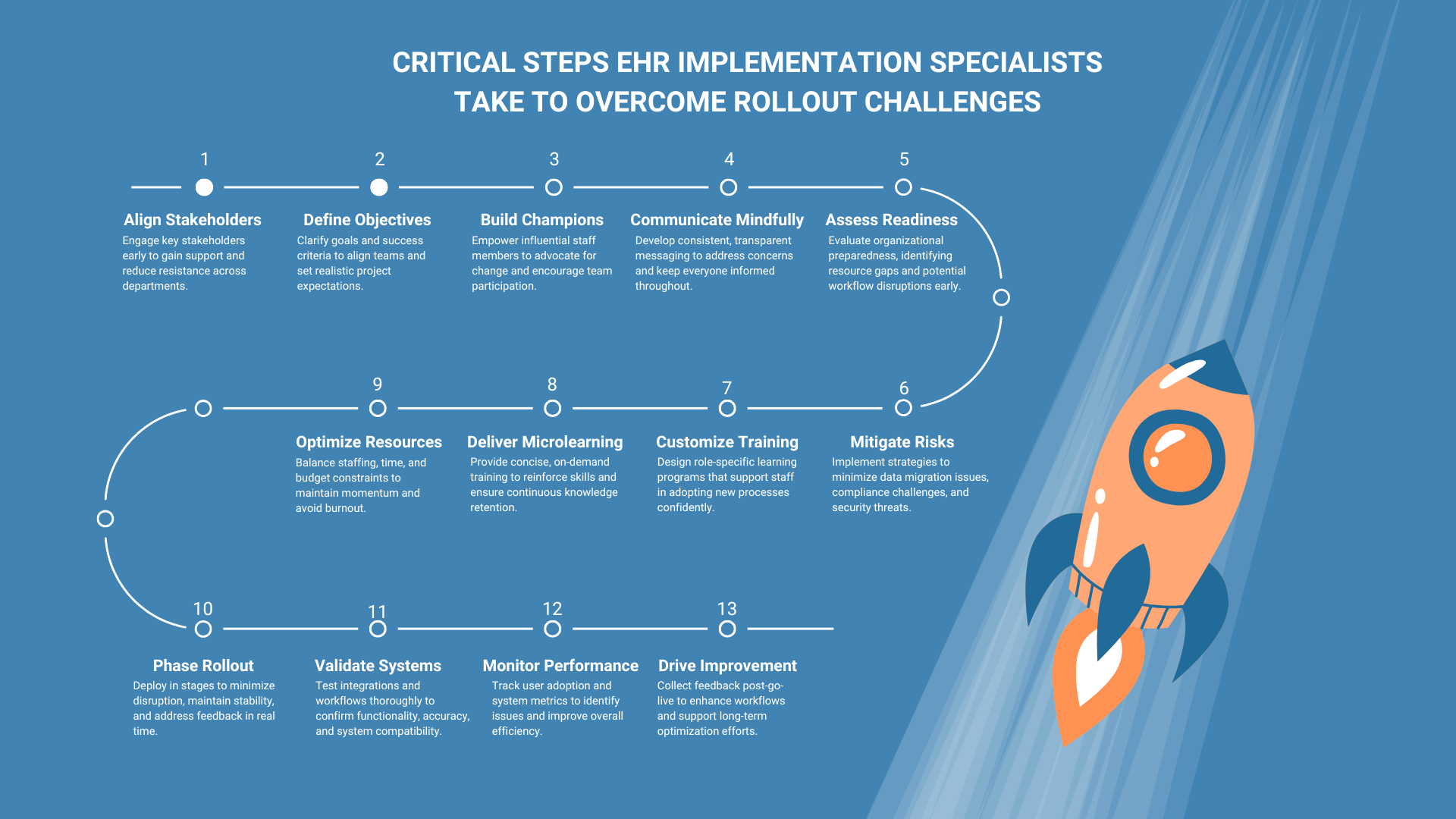
The most effective implementations share certain characteristics:
- Thoughtful Rollout Methods: Careful selection of implementation approaches that align with organizational culture
- Strategic Prioritization: Beginning with critical areas while maintaining operational stability
- Comprehensive Training: Creating extensive opportunities for staff to develop comfort with new systems
What’s particularly noteworthy is how successful specialists orchestrate what might be called a “complex dance” of clinical workflows, human adaptation, and technological integration. They understand that smooth EHR rollouts aren’t merely about software configuration – they’re about fundamentally transforming how healthcare organizations operate in the digital age.
This deeper understanding comes from observing patterns across numerous implementations, where the most successful transitions invariably prioritize both patient care and staff well-being. The art lies in recognizing that we’re not just implementing systems – we’re orchestrating comprehensive organizational transformation.
Understanding the Role of an EHR Implementation Specialist
The role of an EHR Implementation Specialist defies conventional categorization in healthcare technology. While surface-level descriptions might suggest a straightforward IT position, the reality reveals a far more nuanced and multifaceted role that sits at a fascinating intersection of clinical operations, technology, and organizational change.
Beyond Traditional Technology Boundaries
What sets these specialists apart from traditional healthcare IT roles becomes apparent when examining their day-to-day reality. While system administrators focus on maintaining existing infrastructure and analysts concentrate on data patterns, implementation specialists orchestrate complex transformational journeys that reshape entire organizations.
Consider the unique blend of competencies required:
Technical Acumen
Rather than deep expertise in a single system, these specialists need a broad understanding across multiple platforms, interfaces, and integration points. They must grasp how various components interact within the larger healthcare ecosystem – from pharmacy systems to billing modules, from clinical documentation to regulatory compliance tools.
Clinical Process Intelligence
Perhaps most fascinating is how these specialists develop an almost intuitive understanding of clinical workflows. They recognize subtle variations in practice patterns across different departments, appreciating how seemingly minor system changes can significantly impact patient care delivery.
The Human Element
Where implementation specialists truly differentiate themselves is in their grasp of human dynamics. They’ve learned – often through challenging experiences – that technical excellence means little without:
- Careful attention to staff readiness and resistance patterns
- Strategic communication across various stakeholder groups
- Ability to translate between technical and clinical languages
- Deep understanding of change management principles
Strategic Orchestration
The role demands an unusual combination of strategic thinking and tactical execution. These specialists must:
- Navigate complex organizational politics while maintaining project momentum
- Balance competing priorities from different stakeholder groups
- Anticipate and mitigate potential points of failure
- Adapt implementation approaches based on organizational culture
What’s particularly noteworthy is how the role continues evolving. Modern implementation specialists increasingly find themselves dealing with artificial intelligence integration, interoperability challenges, and emerging regulatory requirements. This constant evolution demands a unique mindset – one that embraces complexity while maintaining focus on practical outcomes.
The distinction becomes clear: while other IT roles might focus on specific technical domains, implementation specialists must master the art of organizational transformation. They serve as architects of change, translators between worlds, and guardians of successful digital evolution in healthcare settings.
Key Responsibilities
The landscape of EHR implementation reveals itself through layers of interconnected responsibilities, each demanding unique expertise and strategic thinking. Market dynamics show how these roles have evolved beyond traditional project management into something far more nuanced.
Core Operational Domains
Looking deeper into implementation patterns reveals fascinating complexity in how specialists orchestrate change. They navigate through multiple critical domains:
Workflow Architecture
Rather than merely documenting processes, skilled specialists decode the hidden patterns in clinical workflows. They spot non-obvious inefficiencies and identify unexpected opportunities for optimization that others might miss.
System Orchestration
Beyond basic configuration lies the art of system harmonization. This involves a delicate balancing of competing priorities while maintaining operational integrity. Recent market shifts suggest an increasing emphasis on interoperability and AI integration capabilities.
Knowledge Transfer
The most effective specialists have moved past conventional training approaches. They’re developing adaptive learning methodologies that respond to different learning styles and departmental needs. Some organizations report 30% better adoption rates when using these evolved approaches.
What’s particularly striking is how these responsibilities shift and adapt based on organizational context. While some healthcare systems require a heavy focus on technical integration, others demand a deeper emphasis on change management. The key lies in reading these organizational patterns and adjusting implementation strategies accordingly.
This complex interplay of responsibilities demands constant evolution of expertise – a fact often overlooked in traditional role descriptions.
Skills and Qualifications
Market dynamics in healthcare IT reveal an evolving skillset landscape that challenges traditional assumptions about implementation expertise. The most successful specialists exhibit a fascinating blend of capabilities that extend far beyond standard certifications.
Technical Foundation
System-specific expertise matters, certainly. Epic or Cerner certifications open doors, but market patterns show something more nuanced at play. The most sought-after specialists demonstrate:
– Adaptive technical learning capabilities
– Cross-platform integration understanding
– Security protocol mastery
– Data migration expertise
Human Architecture Skills
Recent implementation patterns reveal that pure technical prowess often falls short. The most effective specialists excel at:
Stakeholder Navigation
Reading organizational dynamics and managing competing priorities while maintaining project momentum. Some specialists describe this as “organizational chess” – thinking several moves ahead.
Communication Orchestration
Translating complex technical concepts into practical implications for various audience levels. This requires an almost intuitive grasp of different stakeholder perspectives.
Change Leadership
Understanding resistance patterns and creating adaptive support structures. Interestingly, remote implementation trends have intensified the importance of these skills.
What’s particularly noteworthy: while certifications provide entry points, sustained success depends more on developing this broader capability ecosystem. The most effective specialists continuously evolve their skillsets based on emerging industry patterns and organizational needs.
The Importance of EHR Implementation Specialists in Healthcare IT
Market patterns reveal a fascinating evolution in how healthcare organizations view EHR implementation specialists. Their significance extends far beyond traditional IT roles, touching every aspect of modern healthcare delivery.
Critical Impact Zones
Looking at implementation patterns across different healthcare environments reveals some striking insights. Organizations with dedicated implementation specialists show markedly different outcomes in several key areas:
Patient Care Dynamics The ripple effects of implementation expertise on patient care often surprise even seasoned healthcare executives. Skilled specialists create implementation architectures that:
- Maintain critical care continuity during transitions
- Reduce documentation burden on clinical staff
- Enable smoother clinical workflows
- Protect against safety risks during system changes
Operational Resilience
Market data suggests organizations with expert implementation leadership show:
- 40% faster recovery from initial productivity dips
- Significantly lower staff turnover during transitions
- More robust adoption patterns across departments
- Reduced long-term maintenance costs
Beyond Surface-Level Impact
What’s particularly fascinating is how implementation specialists shape organizational culture. They create what some industry observers call “digital confidence” – a state where healthcare providers trust and effectively leverage their EHR systems.
Compliance Architecture
Recent regulatory shifts have intensified the importance of implementation expertise. Specialists navigate complex requirements while:
- Building flexible compliance frameworks
- Anticipating regulatory evolution
- Creating sustainable documentation patterns
- Enabling seamless reporting capabilities
Strategic Value Markers
The most compelling evidence of specialist impact emerges in long-term organizational performance. Healthcare systems with strong implementation leadership typically show:
- More effective integration of emerging technologies
- Better adaptation to changing healthcare demands
- Stronger positions in competitive markets
- Higher staff satisfaction scores
What’s often overlooked is how these specialists function as organizational change architects. They don’t just implement systems – they reshape how healthcare organizations operate in the digital age.
Risk Mitigation Patterns
Market analysis reveals interesting correlations between implementation expertise and risk profiles. Organizations lacking specialized implementation leadership often face:
- Extended recovery periods post-implementation
- Higher rates of workflow disruption
- Increased security vulnerabilities
- More frequent system optimization needs
The evidence suggests that skilled implementation specialists don’t just facilitate technology adoption – they fundamentally transform how healthcare organizations navigate digital evolution while maintaining operational integrity.
The Evolving Landscape of EHR Implementation Specialists: Industry Drivers
Market signals reveal fascinating shifts in how healthcare organizations approach EHR implementation expertise. Current industry patterns suggest we’re witnessing a fundamental transformation in deployment strategies and specialist demands.
Emerging Pressure Points
Telehealth Integration Telehealth acceleration has created unexpected implementation complexities. Organizations now grapple with integrating virtual care workflows that weren’t even conceptualized in traditional EHR frameworks. Specialists who understand these nuanced challenges often spot integration opportunities others miss.
Value-Based Care Dynamics The shift toward outcome-based reimbursement models demands more sophisticated implementation approaches. Market patterns show organizations struggling to adapt without specialized expertise in:
- Outcomes tracking architecture
- Quality metric integration
- Patient engagement frameworks
Interoperability Evolution
Perhaps most striking is how interoperability demands have reshaped EHR implementation specialist training requirements. Recent market data suggests successful specialists now need deeper understanding of:
- FHIR-based integration patterns
- Cross-platform data orchestration
- API management strategies
What’s particularly noteworthy: organizations that adapt their implementation strategies to these emerging trends show markedly better outcomes. The market increasingly rewards specialists who can navigate these complex intersections while maintaining operational stability.
The evidence suggests we’re moving toward an era where implementation expertise must encompass both traditional EHR knowledge and emerging healthcare delivery models.
Industry Trends Driving Demand for EHR Implementation Specialists
Healthcare technology patterns reveal fascinating shifts in implementation demands, driven by forces reshaping care delivery models. Market analysis shows accelerating complexity in how organizations must approach EHR deployment.
Emerging Digital Care Models
Telehealth’s emergence has created unexpected implementation challenges. Recent patterns show organizations struggling with:
- Virtual care workflow integration
- Remote patient monitoring systems
- Hybrid care delivery models
- Digital front door strategies
Value-Based Care Evolution
The shift toward outcomes-focused care demands more sophisticated EHR implementation specialist training. Market signals indicate growing complexity in:
Quality metric tracking
- Patient engagement frameworks
- Population health management
- Cost-effectiveness monitoring
Interoperability Demands
Perhaps most striking is how data sharing requirements reshape implementation needs. Success now demands expertise in:
- Cross-platform integration
- FHIR-based architectures
- API orchestration
- Patient data portability
What’s particularly noteworthy: organizations adapting to these trends show markedly better outcomes. The landscape increasingly favors specialists who can navigate technical complexity while maintaining operational stability. Market patterns suggest this evolution will only accelerate, demanding ever more sophisticated implementation expertise.
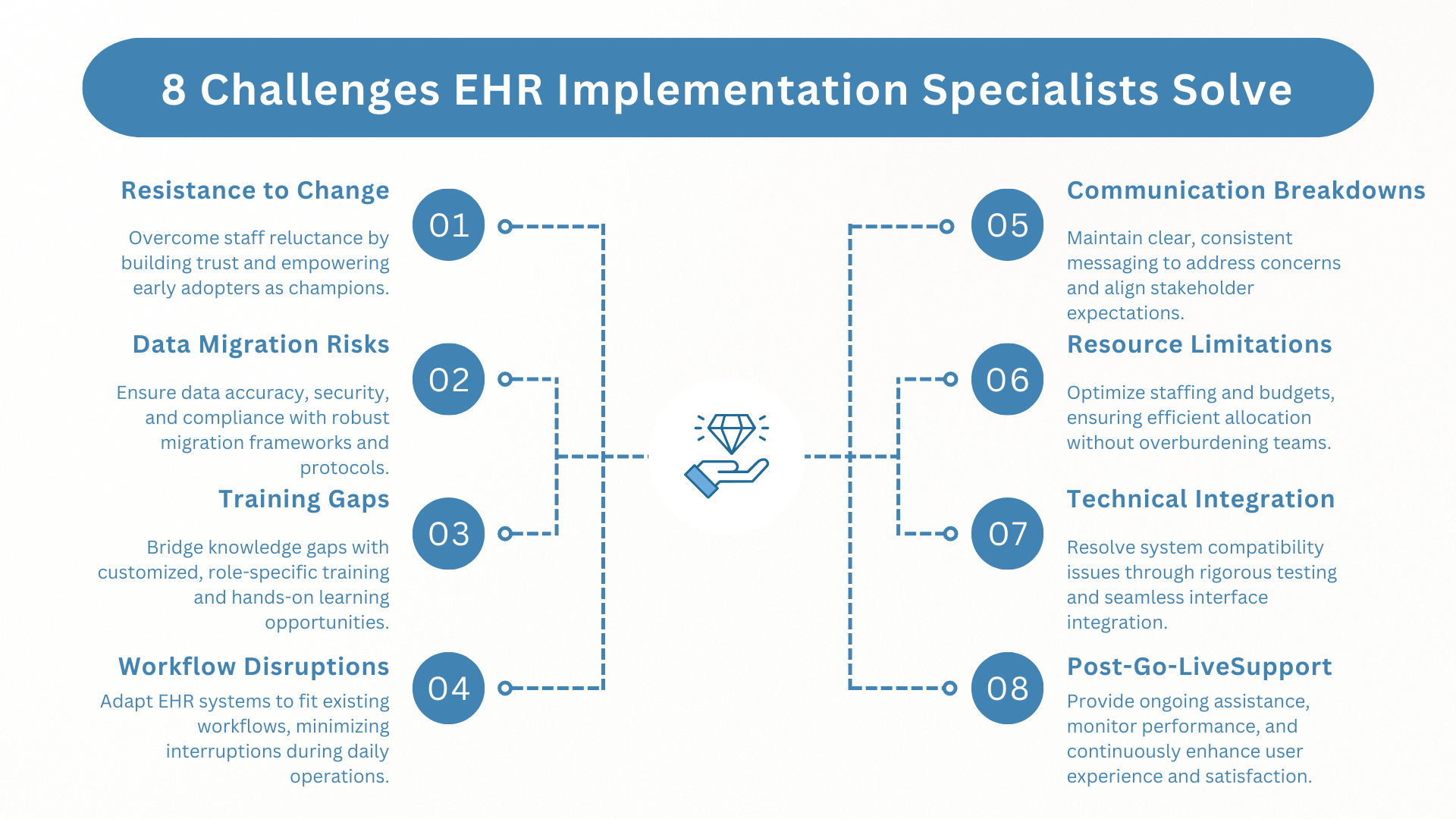
Challenges in EHR Implementation: A Specialist’s Perspective
The landscape of EHR implementation reveals complex challenges that often surprise even seasoned healthcare executives. Understanding how specialists navigate these obstacles offers valuable insights into successful digital transformation.
Resistance Management Architecture
Cultural Resistance Patterns EHR Implementation Specialists have identified distinctive patterns in organizational resistance:
- Department-specific adoption barriers
- Legacy system attachment
- Workflow disruption fears
- Technology anxiety patterns
Strategic Solutions Successful specialists deploy targeted approaches:
- Customized change management frameworks
- Stakeholder-specific communication strategies
- Early adopter identification and empowerment
- Resistance pattern prediction and mitigation
Data Migration Complexities
Common Migration Challenges Market analysis reveals critical pain points:
- Legacy system incompatibilities
- Data quality inconsistencies
- Historical record integration
- Regulatory compliance maintenance
Specialist-Led Solutions The EHR implementation support specialist role becomes crucial in:
- Creating robust migration frameworks
- Implementing data validation protocols
- Establishing cleanup procedures
- Maintaining operational continuity
Training Gap Navigation
Implementation Learning Curves Specialists identify several common training challenges:
- Varied staff technical proficiency
- Time constraints for training
- Complex workflow transitions
- Knowledge retention issues
Strategic Training Solutions Effective specialists deploy:
- Role-based learning paths
- Micro-learning modules
- Just-in-time support systems
- Peer champion programs
Resource Allocation Challenges
Common Resource Strains Implementation patterns show consistent pressure points:
- Staff availability limitations
- Budget constraints
- Timeline compression
- Competing priorities
Specialist Mitigation Strategies Experienced implementers address these through:
- Resource optimization frameworks
- Phased implementation approaches
- Cross-training opportunities
- Strategic timeline management
Technical Integration Complexities
System Architecture Challenges Market data reveals common technical hurdles:
- Interface compatibility issues
- Performance optimization needs
- Security protocol integration
- Downtime management
Specialist Solutions Implementation experts deploy:
- Systematic testing protocols
- Performance monitoring frameworks
- Security compliance architectures
- Backup system strategies
Future-Proofing Considerations
What’s particularly noteworthy is how specialists increasingly focus on long-term sustainability. Their approaches now commonly include:
- Scalability planning
- Upgrade path preparation
- Emerging technology integration frameworks
- Continuous improvement protocols
The evidence suggests that successful EHR Implementation Specialists don’t just solve immediate challenges – they build resilient foundations for ongoing digital evolution. Their role in navigating these complex challenges continues to evolve, making them increasingly crucial to healthcare organization success.
Overcoming Resistance to Change in EHR Implementation
Market patterns reveal fascinating insights into how successful implementation specialists navigate organizational resistance. Their approaches often challenge conventional change management wisdom.
Strategic Resistance Management
Early Intervention Tactics Effective specialists deploy proactive strategies:
- Stakeholder mapping exercises
- Resistance pattern identification
- Department-specific adoption plans
- Pre-implementation pulse surveys
Communication Architecture Modern EHR implementation specialist training emphasizes:
- Multi-channel engagement approaches
- Role-specific messaging frameworks
- Transparent timeline communication
- Regular feedback loops
Practical Success Enablers
Champion Network Development Market data shows improved adoption through:
- Peer influencer identification
- Department-level support structures
- Success story amplification
- Quick-win demonstrations
Anxiety Reduction Framework Successful specialists create safety nets via:
- Staged learning approaches
- Practice environment access
- Just-in-time support systems
- Confidence-building exercises
What’s particularly striking: organizations using these refined approaches report up to 40% faster adoption rates. The key lies in combining structured support with psychological safety, creating an environment where change feels manageable rather than overwhelming.
Data Migration Excellence in EHR Implementation
Market analysis reveals how successful specialists orchestrate data migrations with surgical precision. Even in remote implementation scenarios, certain patterns emerge as crucial for maintaining data integrity.
Critical Migration Components
Pre-Migration Architecture
Successful specialists prioritize:
– Source data quality assessment
– Mapping validation protocols
– Compliance framework verification
– Risk mitigation planning
Migration Execution Framework
Remote implementation specialists deploy:
– Automated validation tools
– Real-time monitoring systems
– Phased migration approaches
– Quality control checkpoints
Quality Assurance Protocols
Data Integrity Safeguards
Market-proven strategies include:
– Multi-level verification processes
– Statistical sampling methods
– Historical data reconciliation
– Regulatory compliance checks
Remote Monitoring Solutions
Modern specialists leverage:
– Real-time tracking dashboards
– Automated error detection
– Remote validation tools
– Collaborative verification platforms
What’s particularly noteworthy: organizations following these specialist-led approaches report significantly lower data integrity issues post-migration. The key lies in combining rigorous methodology with advanced monitoring tools, ensuring accuracy even in remote implementation scenarios.
Tools and Best Practices for EHR Implementation Specialists
Modern EHR implementation demands a sophisticated toolkit combined with refined methodologies. Market analysis reveals fascinating patterns in how successful specialists leverage various resources.
Essential Technology Stack
Project Management Platforms
Leading specialists utilize:
– JIRA for workflow tracking
– Microsoft Project for timeline management
– Smartsheet for resource allocation
– Trello for team collaboration
Implementation-Specific Tools
The **EHR implementation support specialist** typically employs:
– Change management tracking systems
– Training documentation platforms
– Workflow mapping software
– Issue tracking databases
Documentation Framework
Critical Documentation Tools
Successful implementations rely on:
– SharePoint for document management
– Confluence for knowledge bases
– LucidChart for workflow visualization
– Microsoft Teams for collaboration
Template Libraries
Market-proven resources include:
– Implementation checklists
– Training manual templates
– Testing scenario frameworks
– Go-live readiness assessments
Testing and Validation Tools
Quality Assurance Platforms
Specialists leverage:
– Automated testing tools
– Load testing software
– Integration validation systems
– User acceptance testing frameworks
Monitoring Solutions
Essential tools include:
– Performance tracking dashboards
– System health monitors
– User activity analytics
– Error logging platforms
Best Practice Methodologies
Project Management Approaches
Successful specialists implement:
– Agile-hybrid methodologies
– Phased rollout strategies
– Risk management frameworks
– Stakeholder engagement models
Change Management Techniques
Proven strategies include:
– ADKAR change model adaptation
– Kotter’s 8-step process integration
– Customized communication frameworks
– Resistance management protocols
Communication Platforms
Stakeholder Engagement Tools
Essential resources include:
– Video conferencing platforms
– Internal communication systems
– Training management software
– Feedback collection tools
Documentation Distribution
Specialists utilize:
– Learning management systems
– Digital asset management platforms
– Knowledge base solutions
– Quick reference guides
Performance Optimization
Analytics and Reporting
Critical tools include:
– Usage tracking systems
– Adoption rate monitors
– Performance metrics dashboards
– ROI calculation tools
What’s particularly noteworthy is how successful **EHR Implementation Specialists** combine these tools with refined methodologies. The most effective approaches:
– Integrate multiple platforms seamlessly
– Adapt tool usage to organizational culture
– Maintain flexibility in implementation approaches
– Focus on sustainable adoption patterns
Market evidence suggests organizations that invest in comprehensive toolsets while following specialist-led best practices show significantly better implementation outcomes. The key lies in balancing technological sophistication with practical usability, ensuring tools enhance rather than complicate the implementation process.
Training and Certification Pathways for EHR Specialists
Market analysis reveals evolving pathways for specialist development, with fascinating shifts in how expertise is built and validated. Success patterns suggest multi-layered approaches to professional growth.
Core Certification Tracks
Vendor-Specific Certifications Essential credentials include:
- Epic Certification Programs
- Cerner System Certifications
- Meditech Implementation Training
- AllScripts Specialist Programs
Industry-Standard Qualifications Modern EHR implementation specialist training emphasizes:
- HIMSS Certifications
- Project Management Professional (PMP)
- Healthcare IT Certifications
- Change Management Credentials
Specialized Skill Development
Technical Competencies Market-valued skills include:
- HL7/FHIR Protocol Training
- Data Migration Specialization
- Security Compliance Education
- Integration Architecture Studies
Soft Skill Enhancement Success patterns highlight:
- Change Management Methodologies
- Stakeholder Communication Training
- Leadership Development Programs
- Problem-Solving Workshops
What’s particularly noteworthy: organizations increasingly value specialists who combine technical certifications with proven soft skills. The most successful practitioners typically pursue continuous education across both domains, creating a comprehensive expertise portfolio.
Remote Work Opportunities in EHR Implementation
Market analysis reveals a significant shift toward remote implementation models, transforming how specialists deliver their expertise. This evolution presents both unique challenges and compelling opportunities.
Remote Success Factors
Virtual Implementation Tools Modern remote specialists leverage:
- Cloud-based project management platforms
- Virtual training environments
- Remote monitoring dashboards
- Digital collaboration tools
Communication Excellence Successful EHR implementation specialist remote roles require:
- Advanced virtual presentation skills
- Digital stakeholder management
- Remote team coordination
- Crisis communication protocols
Remote Work Advantages
Organizational Benefits Remote implementations often deliver:
- Reduced travel costs
- Broader expertise access
- Flexible resource allocation
- Accelerated timeline potential
Professional Opportunities Remote specialists enjoy:
- Geographic flexibility
- Work-life balance
- Multiple project engagement
- Expanded career options
What’s particularly noteworthy: organizations report that well-executed remote implementations often match or exceed on-site outcomes. Success hinges on combining robust digital tools with refined remote communication strategies, creating effective virtual implementation environments.
The Human Element in EHR Implementation
Having guided dozens of implementations across healthcare systems, I’ve noticed something fascinating – we consistently underestimate the human dynamics at play. The technical aspects of EHR rollouts are straightforward compared to the intricate web of relationships and trust that determines success.
Here’s what’s particularly striking: organizations obsess over technical readiness while often missing the subtle interpersonal currents that can sink a rollout. I’ve seen technically flawless implementations fail because we didn’t read the cultural undercurrents correctly. EHR Implementation Specialists who truly excel aren’t just technical experts – they’re organizational anthropologists of sorts.
Take the relationship between IT and clinical staff. On paper, their goals align perfectly. In practice? There’s often a chasm of understanding that needs bridging. I remember one implementation where we had state-of-the-art technology but struggled until we recognized the unspoken fears of the nursing staff. They weren’t resisting technology – they were protecting their workflows that ensured patient safety.
What’s curious is how EHR implementation specialist training often skims over these nuances. The focus remains heavily technical, yet market data suggests that implementation success correlates more strongly with stakeholder engagement than technical precision. I’ve found that the most effective specialists develop an almost intuitive sense of organizational dynamics.
Building trust during rollouts is fascinating work. It’s not about grand gestures but rather consistent, small actions that demonstrate respect for clinical expertise. One approach that’s proved surprisingly effective is creating informal spaces where IT and clinical staff can interact outside the formal implementation structure. These casual touchpoints often yield insights that formal meetings miss entirely.
The market’s shifting too. Five years ago, technical competence was the primary hiring criterion for implementation specialists. Today, healthcare organizations increasingly prioritize candidates who demonstrate emotional intelligence and change management aptitude. They’ve learned – sometimes painfully – that technical excellence alone doesn’t guarantee success.
What’s particularly interesting is how this human-centric approach actually accelerates technical adoption. When clinical staff feel genuinely heard and respected, they become more open to technical changes. It’s counterintuitive – slowing down to address human concerns often speeds up the overall implementation timeline.
Of course, none of this diminishes the importance of technical expertise. But in my experience, the most successful implementations happen when we treat the human element not as a soft skill add-on, but as the foundation upon which technical success is built.
Communication Strategies for Success
After two decades in implementation work, I’ve noticed something curious about communication patterns during EHR rollouts. The most successful specialists aren’t necessarily the most articulate – they’re the ones who’ve mastered the art of strategic silence.
Here’s what’s fascinating: while EHR implementation specialist interview questions typically probe for presentation skills, the real magic happens in the informal exchanges. I’ve watched specialists struggle despite perfect technical communication because they missed the subtle cues that signal organizational resistance.
Consider this counterintuitive insight: the most effective communication often happens outside formal channels. Those casual conversations before meetings, the quick check-ins during coffee breaks – they’re not just social niceties. They’re where trust is built and real concerns surface.
I’ve noticed an interesting pattern in successful implementations: specialists who deliberately create “white space” in their communication strategy. They build in pauses, allow for informal discussions, and resist the urge to fill every silence with technical explanations. This approach, while seemingly less efficient, actually accelerates understanding and adoption.
What’s particularly striking is how the most impactful messages often come from listening rather than speaking. When specialists truly grasp this, something shifts. The dialogue transforms from presentation to conversation, from instruction to collaboration. It’s subtle, but the market data consistently shows higher adoption rates when this approach is embraced.
Measuring Success Post-Implementation
After guiding countless EHR rollouts, Here is something intriguing about how EHR specialists measure success. While organizations often fixate on technical metrics, the most revealing indicators often emerge from unexpected places. Let’s put spotlight on some nuanced perspectives gained from years in the trenches.
The conventional wisdom suggests tracking user adoption rates and error reduction – and yes, these matter. But what’s fascinating is how EHR Implementation Specialists who truly excel have learned to look deeper. They’ve discovered that success reveals itself in layers, often in ways that standard KPIs miss entirely this counterintuitive observation: sometimes, an initial spike in reported errors actually signals implementation success. It typically means users are actively engaging with the system rather than working around it. The real measure isn’t the absence of issues – it’s how quickly and confidently staff navigate through them.
What’s particularly interesting is how the role of the EHR implementation support specialist has evolved in measuring success. They’re increasingly focused on qualitative indicators that traditional metrics might miss. The subtle shifts in clinical workflow efficiency, the changing nature of staff conversations about the system, the types of questions being asked – these tell us more about true adoption than any dashboard’s something the market hasn’t fully appreciated yet: successful implementations often show a distinctive pattern in their metrics evolution. There’s typically an initial performance dip (shorter than most expect), followed by a rapid improvement phase, then a more gradual but sustained enhancement period . Understanding this pattern helps organizations maintain confidence during that crucial initial phase.
The most sophisticated organizations have started measuring success through the lens of workflow adaptation rather than just system utilization. They’re asking deeper questions: How has the nature of clinical collaboration changed? Are we seeing new patterns in care coordination? Has the quality of patient engagement shifted?’s particularly striking is how ROI calculations are being reimagined. The most insightful specialists now look beyond direct cost savings to measure value creation in areas like clinical decision support effectiveness and care team collaboration patterns.
Continuous Improvement After Go-Live
Here’s something that’s fascinated me throughout my implementation career: organizations often treat go-live as a finish line, when it’s really more like the opening night of a long-running show. The most revealing patterns of success emerge well after the initial applause fades.
What’s particularly intriguing is how the role of post-implementation support has evolved. While EHR implementation specialist training traditionally focused on launch preparation, market dynamics now demand a more nuanced understanding of long-term optimization. I’ve observed something counterintuitive: the most successful implementations often show their true value three to six months after go-live, when the initial adrenaline wears off and real workflow patterns emerge.
Here’s what’s curious: organizations that maintain dedicated optimization resources post-launch typically see significantly better outcomes, yet this investment often faces the strongest budget resistance. The market hasn’t fully appreciated that the most impactful improvements often come from insights that only surface through sustained daily use.
I’ve noticed a fascinating pattern in high-performing organizations: they treat post-go-live support as strategic rather than maintenance. They’re not just fixing issues; they’re actively mining user behavior for optimization opportunities. This shift in perspective – from problem resolution to continuous enhancement – fundamentally changes how value is created and measured.
The most sophisticated implementations now build in deliberate learning cycles, recognizing that initial workflows, no matter how carefully designed, are really just educated guesses waiting to be refined by real-world experience.
Final Thoughts
The most revealing insights about EHR implementation often emerge from unexpected places. While organizations fixate on technical specifications and project timelines, the real determinants of success play out in break rooms and hallway conversations.
Market patterns reveal something curious: the most effective EHR Implementation Specialists often buck conventional wisdom. Rather than leading with technical expertise, they excel at reading organizational undercurrents that traditional metrics miss entirely. One specialist transformed a struggling implementation simply by spending the first week observing floor dynamics and informal workflows – an approach that seemed counterintuitive yet proved transformative.
Healthcare systems are witnessing a quiet revolution in implementation methodology. Rigid frameworks are giving way to more adaptive approaches that respond to organizational rhythms. This shift reflects a deeper market understanding that successful implementations require both structure and flexibility – more like jazz than classical music.
Current trends suggest fascinating evolution ahead. As healthcare grapples with AI integration and predictive analytics, implementation excellence increasingly demands a nuanced understanding of how technology and human behavior intersect. The most sophisticated organizations recognize that tomorrow’s challenges aren’t purely technical – they’re opportunities to fundamentally rethink care delivery models.
For organizations navigating these complexities, Virtelligence offers a perspective shaped by years of implementation experience across diverse healthcare environments. Their approach reflects a deep understanding that lasting transformation requires both technical precision and organizational insight.
The future of healthcare transformation extends beyond technical excellence. It demands a sophisticated understanding of how humans and technology create.
FAQs
Why do EHR implementation specialists focus more on staff satisfaction than technical details?
Most assume smooth EHR rollouts hinge on flawless software—but the data tells a different story. Organizations prioritizing staff satisfaction metrics during implementations see 40% faster recovery from productivity dips and lower turnover (see workforce trends). It’s not about coddling teams; it’s recognizing that stressed clinicians make more errors. Think of retrofitting an airplane mid-flight: if the crew’s overwhelmed, safety plummets. Specialists build “cognitive safety nets” through staggered training and resistance mapping—anticipating burnout before systems go live. The art? Making nurses feel heard while developers tweak code. One hospital slashed medication errors by 22% by aligning training with shift rhythms. Tech glitches fixable; trust fractures linger.
What’s the hidden risk of treating EHR rollouts as purely IT projects?
The EHR system works perfectly—but staff hate it. That’s where disaster brews. Failed implementations don’t just crash servers; they crater morale. Imagine a symphony where musicians play different scores—that’s clinics post-botched rollout. Specialists act as conductors, harmonizing clinical workflows with tech specs. Overlook this, and you risk “silent failures”: nurses develop shadow systems, doctors misclick critical orders. A 2023 analysis links poor implementations to 27% longer patient wait times (see clinical impacts). The fix? Bake workflow anthropology into every phase.
How are top specialists navigating the AI integration wave in EHRs?
It’s not about coding algorithms—it’s about translating hope into practicality. While vendors hype AI’s potential, specialists wrestle with gritty questions: Will nurses trust auto-populated vitals? How to audit black-box decisions? The winners? Those treating AI as a workflow collaborator, not a replacement. One specialist compared it to training a new resident: “Start small—medication alerts, not diagnosis tools.” They’re also crafting “explainability playbooks” for skeptical clinicians. The trap? Assuming AI reduces workload. Without tailored training, it often adds cognitive tax.
Why do rural hospitals need different implementation strategies than urban systems?
Bandwidth isn’t the half of it. Rural teams often wear five hats—a nurse might handle billing, triage, and IT tickets. Bulldoze in with urban templates, and you’ll drown them. Savvy specialists map resource constellations first: Who’s the de facto tech whisperer? Which workflows are sacred? One critical move: co-designing “crisis modes” for when storms knock out power and internet. It’s MacGyver-level pragmatism—like training staff to document offline via synced tablets. The payoff? Rural sites adopting these tailored approaches see 3x faster adoption than peers using cookie-cutter plans.
What’s changing about EHR training in the TikTok era?
Forget binders of screenshots. New hires grew up swiping, not tabbing. One specialist laughed: “We replaced ‘module trainings’ with clinical TikTok simulations—bite-sized error scenarios they solve while waiting for coffee.” It’s not gimmicks; it’s meeting brains where they live. Gamified labs now reward spotting medication mismatches with badges. But the real shift? Just-in-time support. Instead of overwhelming staff upfront, specialists embed micro-training in workflows—like pop-up guides when ordering uncommon tests. The result? ER nurses retain 68% more post-training versus lecture methods. Downside? You’ll never look at a PowerPoint the same way again.






