Introduction
Understanding EHR Investments: Why Hospitals are Turning to Epic
In today’s fast-paced, technology-driven healthcare environment, hospitals are increasingly moving towards Electronic Health Record (EHR) systems to enhance patient care and streamline operations. One of the most well-known EHR suppliers is Epic Systems which has made a name for itself as a top option for numerous healthcare facilities and healthcare providers. But how much does Epic cost for a hospital? Every hospital’s decision to invest in this platform is based mostly on this question. Whereas the benefits of EHR systems like Epic are clear, the financial commitment required is significant which makes it essential for hospitals to fully understand the costs involved.
Epic is designed to integrate accurately into various aspects of hospital operations which schedule billing, telehealth solutions and lab results. There are many aspects in the Epic system that go beyond those of standard medical records. Hospitals are choosing Epic not only because of its inclusive feature set but also due to its reputation for improving patient outcomes, meeting regulatory requirements and enhancing data security. However, before making this decision, understanding how much does Epic cost for a hospital in both the short and long term is crucial for hospital administrators and decision-makers.
Importance of Knowing the Costs: Balancing Cost and Quality in Healthcare Tech
When hospitals evaluate EHR systems, the primary factors are not only the functionalities and advantages but also the price. Knowing how much does Epic cost for a hospital is fundamental because, while the platform offers robust and diverse capabilities, it comes with a hefty price tag that varies depending on the size and needs of the hospital. Costs typically include initial implementation fees, ongoing maintenance, training, and potential upgrades, all of which can add up quickly.
The investment in Epic can be a balancing act for hospitals—between cost and the quality of care delivered. While the initial expenditure can be high, many hospitals justify this by pointing to the improved operational efficiencies, enhanced patient care, and long-term cost savings that Epic can bring. This is why it is essential for hospitals to conduct a thorough cost-benefit analysis before implementing Epic which ensures that they fully understand how much does Epic cost for a hospital and whether the investment aligns with their financial goals and patient care objectives.
Additionally, hospitals must consider the total cost of ownership (TCO), which includes not only the upfront licensing fees but also the continuous costs associated with maintaining the system. For example, ensuring data integrity, compliance with health regulations, and updating the system as new features and requirements emerge will incur additional expenses. Thus, the question of how much does Epic cost for a hospital becomes an ongoing consideration, not just a one-time decision.
Overview of Epic Systems: A Leader in the Electronic Health Record (EHR) Market
Overview of Epic Systems
- Founded in 1979 – Epic Systems is a leading player in the Electronic Health Record (EHR) market.
- All-inclusive Platform – The company provides a strong platform for hospitals, clinics, and outpatient centers.
- Tailored Solutions – Epic’s software is scalable, designed to meet the specific needs of different types of healthcare facilities.
How Much Does Epic Cost for a Hospital?
- Key Question – One of the primary concerns for hospital administrators is understanding how much does Epic cost for a hospital before deciding to implement the system.
- Initial Investment – Hospitals need to evaluate how much does Epic cost for a hospital in terms of upfront investments like licensing fees, hardware, software, and labor costs.
- Basic Implementations – Even smaller hospitals must ask how much does Epic cost for a hospital when choosing more streamlined versions of the system.
Scalable Solutions for Different Hospitals
- Large Academic Centers – Larger medical centers often need advanced customizations, affecting how much does Epic cost for a hospital on a larger scale.
- Community Hospitals – Smaller facilities may lower how much does Epic cost for a hospital by opting for fewer features and less complexity.
Upfront Costs of Implementation
- Licensing and Hardware – Initial costs are driven by software licenses and hardware setups, forming a major part of how much doesEpic cost for a hospital.
- Labor Costs – Customizing the system involves labor, and this is a significant factor when determining how much does Epic cost for a hospital.
- Training Expenses – Training staff to use Epic adds another layer to how much does Epic cost for a hospital, particularly for large-scale implementations.
Ongoing Costs of Epic
- Maintenance and Support – Once implemented, hospitals need to consider how much does Epic cost for a hospital in ongoing expenses such as system maintenance and technical support.
- System Updates – Periodic updates can increase how much does Epic cost for a hospital, making these expenses essential to consider for long-term planning.
- Compliance Costs – Hospitals must comply with regulatory standards, adding to how much does Epic cost for a hospital over time.
Epic’s Market Dominance
- Integrated Solutions – Epic dominates the market by offering solutions that enable cooperation across different departments, but hospitals must assess how much doesEpic cost for a hospital to ensure financial feasibility.
- Future Demands – Investing in Epic requires hospitals to evaluate how much does Epic cost for a hospital not only today but also in terms of its ability to meet future needs.
1. The Role of EHR Systems in Modern Healthcare
Digital Transformation in Healthcare: The Shift from Paper to Digital
- The Shift to EHR Systems – The healthcare industry has shifted from paper-based records to advanced Electronic Health Record (EHR) systems like Epic.
- Improved Patient Care – EHR systems allow healthcare providers to access patient information in real-time, improving the quality of care and operational efficiency.
Adoption of EHR Systems like Epic
- Modernizing Workflows – Hospitals are adopting EHR systems like Epic to streamline processes, but a common question is, how much does Epic cost for a hospital?
- Key Financial Consideration – As healthcare facilities move toward digital transformation, understanding how much does Epic cost for a hospital becomes crucial for budget planning.
Benefits of Moving from Paper to Digital
- Advantages of Digital Records – Digital health records are more secure, accessible, and manageable compared to paper records, which are prone to errors and inefficiencies.
- Reduced Human Error – EHR systems reduce the risks associated with misplacement and retrieval of patient data, which were common issues with paper records.
Cost Considerations in Implementing Epic
- Beyond Paper – Implementing an EHR system like Epic involves more than just switching from paper—it includes installation, training, hardware upgrades, and long-term maintenance.
- How Much Does Epic Cost for a Hospital? Understanding the full scope of implementation costs is vital for hospitals looking to adopt Epic during their digital transformation.
Epic Systems? A Breakdown of Epic’s Functionalities and Offerings
Epic Systems: A Leading EHR Platform
- Global Trust – Epic Systems is one of the largest and most trusted Electronic Health Record (EHR) platforms globally, used by leading hospitals and healthcare organizations.
- Comprehensive Suite – Epic offers a wide range of tools, including patient management, medical records, clinical systems, billing, and telehealth services.
Customization and Workflow Integration
- Seamless Workflow – Epic’s features are designed to streamline hospital operations by enabling smooth communication between departments, ensuring efficient care coordination.
- Customizable to Needs – Hospitals can tailor Epic to fit their specific needs, from department-specific templates to advanced data analytics that enhance operational performance.
How Much Does Epic Cost for a Hospital?
- Critical Question – The cost of adopting Epic is a major consideration for hospitals, prompting administrators to ask, how much does Epic cost for a hospital?
- Complex Factors – The answer to how much does Epic cost for a hospital depends on factors like the hospital’s size, customization needs, and scalability.
Scalability and Cooperation
- Adaptability – One of the reasons hospitals choose Epic, despite wondering how much does Epic cost for a hospital, is its ability to scale to different healthcare facility sizes.
- Interoperability and Cooperation – Epic’s system boosts data sharing across departments, which improves collaboration and continuity of care and makes it a worthwhile investment despite how much does Epic cost for a hospital.
Cost vs. Value
- Investment Worth Making – Epic’s reliability, scalability, and interoperability make it a preferred choice for hospitals, but understanding how much does Epic cost for a hospital remains a vital step before adoption.
- Balancing Needs and Budget – While the benefits are clear, the financial implications of how much does Epic cost for a hospital must be carefully weighed to ensure it fits within both current needs and long-term goals.
How EHRs Improve Patient Care: Benefits such as Accuracy, Accessibility, and Efficiency
- Improving Patient Care – One of the main reasons hospitals adopt EHR systems like Epic is to improve patient care as well as to boost, increase and improve outcomes such as accessibility, efficiency and accuracy of the healthcare system. Moreover, healthcare providers and organizations can profit from electronic health records in a number of ways, including knowing their organization’s efficiency.
- Financial Considerations – As hospitals assess these benefits, they also need to evaluate how much does Epic cost for a hospital to determine whether the value aligns with the financial investment required.
Accuracy in Medical Records
- Error Reduction – EHR systems like Epic minimize errors common in paper records, such as illegible handwriting or misinterpreted information.
- Better Decision-Making – Clear, organized, and easily accessible digital records help healthcare providers make more informed decisions, improving patient outcomes.
- Cost Factor – To take advantage of these accuracy improvements, hospitals must first assess how much does Epic cost for a hospital, which includes expenses like staff training.
Accessibility of Patient Information
- Real-Time Access – Epic allows healthcare providers to access patient records anytime and from any location, improving timely care, particularly in emergencies.
- Continuity of Care – Seamless data sharing across departments ensures consistent care throughout a patient’s treatment journey.
- Financial Implications – While the accessibility benefits are clear, hospitals must evaluate how much does Epic cost for a hospital to implement these advanced features and plan their budgets accordingly.
Boosting Operational Efficiency
- Automation of Tasks – Epic automates administrative tasks like billing, scheduling, and record-keeping, reducing manual errors and freeing up time for healthcare professionals to focus on patient care.
- Time Savings – The increased efficiency of hospital operations contributes to better patient care and smoother workflows.
- Cost vs. Savings – The decision to implement Epic often comes down to how much does Epic cost for a hospital and whether the time and cost savings justify the investment in the long term.
Balancing Costs and Benefits
- Significant Benefits – EHR systems like Epic offer substantial advantages, including improved accuracy, better accessibility, and greater efficiency in hospital operations.
- Cost Assessment – However, hospitals must carefully assess how much does Epic cost for a hospital, ensuring the financial investment is justified by the potential benefits to patient care and operational efficiency.
2. Why Hospitals Choose Epic: A Deep Dive
Reputation in the Industry: Epic’s Standing Among Healthcare Institutions
- Epic’s Strong Reputation – Epic Systems has earned a reputation as one of the most trusted and widely used Electronic Health Record (EHR) platforms in healthcare.
- Trusted by Leading Hospitals – Hospitals across the U.S. and globally choose Epic due to its reliability, scalability, and positive impact on clinical outcomes.
Epic’s Key Attributes
- Decades of Experience – Epic’s reputation is built on years of experience, robust system design, and continuous innovation in the healthcare field.
- Decision Factors – Despite its strong standing, hospitals need to carefully assess how much does Epic cost for a hospital to ensure the investment aligns with their budget and needs.
Preferred by Large Healthcare Institutions
- Managing Complicated Information – Epic’s comprehensive features make it ideal for complex healthcare environments which enhance its credibility in the market.
- Cost Consideration for Smaller Hospitals – For smaller hospitals, a crucial question is how much does Epic cost for a hospital of their size, as costs can vary based on specific needs and capabilities.
Prioritize Enhancing Patient Results
- Interoperability – Epic is known for improving patient outcomes and fostering cooperation between hospitals and clinics which further cement its reputation in the industry.
- Balancing Costs with Benefits – While Epic is highly regarded, the costs are significant. Hospitals must evaluate how much does Epic cost for a hospital in comparison to the benefits it provides in terms of performance, functionality, and innovation.
Industry Trust and Financial Considerations
- Epic’s Strong Market Position – Epic’s standing in the healthcare industry is supported by its reputation for reliability, scalability, and improving patient outcomes.
- Critical Financial Assessment – Despite its strong reputation, hospitals must consider how much does Epic cost for a hospital and weigh the benefits against the financial investment before making.
Features that Set Epic Apart: Usability and Advanced Analytics
One of the main reasons hospitals choose Epic is its rich feature set, which distinguishes it from other EHR systems. When evaluating how much does Epic cost for a hospital, it is important to understand the value behind these features and how they improve hospital operations and patient care.
Usability: User-Friendly Interface and Training Requirements
- User-Centered Design – Epic is designed with usability in mind, offering a user-friendly interface that simplifies system navigation for physicians, nurses, and administrative staff.
- Regulated Workflows – The system’s structured workflows enable healthcare providers to access patient information and document care more efficiently, promoting coordinated treatment plans.
- Training Costs – Despite its user-friendly nature, hospitals must invest in training their staff to use Epic effectively, which is why understanding how much does Epic cost for a hospital includes factoring in expenses related to training and onboarding.
Interoperability: Seamless Data Sharing Across Providers
- Connecting Healthcare Providers – One of Epic’s standout features are its interoperability, enabling secure data sharing across hospitals, clinics, and specialists.
- Continuity of Care – This collaboration ensures that patient information can be shared accurately between different providers which leads to better continuity of care, reduced duplicative testing, and fewer diagnostic errors.
- Customization Costs – To leverage Epic’s harmony, hospitals must consider how much does Epic cost for a hospital in terms of the implementation and customization required to support these interoperable workflows.
Advanced Analytics: Data-Driven Decision Making
- Actionable Insights – Epic offers advanced data analytics tools that provide hospitals with insights to improve clinical and operational performance.
- Improving Efficiency and Care – Hospitals can use Epic’s analytics for resource planning, population health management, and enhancing patient care while reducing overall costs.
- Cost of Advanced Features – While the advanced analytics capabilities are a major selling point, hospitals must evaluate how much does Epic cost for a hospital to implement and maintain these features as part of their overall financial planning.
Balancing Usability, Interoperability, and Costs
- Comprehensive Benefits – Epic’s user-friendly interface, compatibility, and advanced analytics offer hospitals powerful tools to improve efficiency and patient care.
- Financial Considerations – However, hospitals must carefully consider how much does Epic cost for a hospital, taking into account training, implementation, customization, and ongoing maintenance, to ensure they maximize the value of the system.
3. Initial Costs of Implementing Epic Systems
Cost Breakdown for a Typical Hospital: Software Licensing, Hardware, and Infrastructure
When deciding to implement Epic Systems, hospital administrators must carefully evaluate the overall costs involved. How much does Epic cost for a hospital varies based on several factors, including software licensing, hardware requirements, and infrastructure improvements. Knowing these expenses is crucial to figuring out whether Epic fits the hospital’s spending plan and objectives as well as how much does Epic cost for a hospital.
Software Licensing
- Licensing Fees – The most significant initial cost comes from Epic’s software licensing fees. These costs for large hospitals might vary from $500,000 to more than $3 million, contingent upon the hospital’s size and particular requirements.
- Subscription Model – Epic typically uses a subscription-based model, meaning hospitals not only face upfront licensing costs but also recurring fees for software maintenance and updates.
- Smaller Hospitals – Even smaller community hospitals must consider how much Epic does cost for a hospital of their size, factoring in lower licensing fees but still substantial recurring expenses.
Hardware and Infrastructure
- Hardware Upgrades – To support Epic’s robust system, hospitals often need to invest in new hardware, including servers, data storage systems, and workstations. Depending on the infrastructure of the hospital, the cost of these hardware changes might vary from several hundred thousand to millions of dollars.
- Larger Hospitals – Larger hospitals that require extensive server and storage upgrades may incur costs exceeding $1 million, particularly if existing systems are outdated or insufficient to handle the software demands.
Network Infrastructure
- Data Handling Requirements – Epic requires a strong network infrastructure to manage large volumes of data. Hospitals can maintain efficient and safe operations while making investments in data security systems, redundancy features.
- Security and Redundancy – Given the sensitive nature of healthcare data, investments in data encryption, cybersecurity, and redundant network systems are essential, potentially adding hundreds of thousands of dollars to the overall cost.
- Cost of Upgrades – The expense of upgrading network infrastructure varies depending on existing systems but can contribute significantly to how much does Epic cost for a hospital, particularly for facilities with outdated or underperforming networks.
Total Initial Investment
- Cost Range – The total upfront cost for implementing Epic can vary greatly. Smaller hospitals might face an initial investment of around $1 million. While large health systems can see costs exceeding $10 million including network infrastructure improvements, hardware upgrades, and software licensing.
- Long-Term Savings – While the initial costs may be high, hospitals should also consider potential long-term savings through improved operational efficiency, reduced administrative errors, and better patient care coordination.
Assessing Total Costs
- Comprehensive Investment – When evaluating how much does Epic cost for a hospital, administrators must factor in software licensing, hardware, and network infrastructure. Although this initial financial outlay is necessary, over time it may result in notable gains in efficiency and quality of care.
- Budgeting for the Future – In addition to upfront costs, hospitals should plan for recurring fees associated with licensing, maintenance, and system updates to fully leverage the benefits of Epic in the long term.
Training and Onboarding Expenses: Ensuring Staff Are Prepared to Use the System
One of the most important aspects of implementing Epic is ensuring that hospital staff are fully trained and ready to use the system efficiently. Hospitals must receive the appropriate training in order to fully profit from the platform. Therefore, it is an important factor when evaluating how much does Epic cost for a hospital.
Training Costs
- Comprehensive Training – Epic is a sophisticated platform, and staff at all levels, including doctors, nurses, administrative personnel, and IT staff, must undergo extensive training. Hiring Epic-certified trainers and paying for costs like software, training materials, and occasionally travel for specialized sessions are the usual steps in this procedure.
- Cost Range – Training costs can range from $500,000 to over $1 million, depending on the hospital’s size and the number of employees involved. Larger hospitals or those with multiple departments requiring specialized training may face higher costs. As a key component of how much does Epic cost for a hospital, this expense cannot be overlooked.
- Critical Investment – Investing in proper training ensures that staff are proficient in using Epic, reducing the risk of errors and inefficiencies. Insufficient funding for training may lead to system underuse that can affect or impact the hospital’s overall performance.
Onboarding and Workflow Adjustments
- Transition Costs – As staff adapt to Epic, hospitals often need to modify workflows, which can temporarily disrupt regular operations. Employees may be less productive during this onboarding time as they become used to the new system.
- Temporary Staffing Needs – Some hospitals may also hire temporary staff to cover for full-time employees attending training sessions, which adds to the indirect costs. These disruptions and adjustments should be considered when assessing how much does Epic cost for a hospital.
- Indirect Expenses – Reduced productivity during the initial phase, coupled with operational adjustments, may create additional indirect costs that hospitals must factor into their budget.
Ongoing Training and Updates
- Continuous Learning – As Epic evolves with new features and regulatory changes, hospitals need to provide ongoing training for their staff to stay current with the system’s updates.
- Recurring Costs – The necessity of periodic retraining adds to the total cost of ownership over time, making it a factor when considering how much does Epic cost for a hospital in the long run. Ongoing training guarantees that employees stay knowledgeable and productive which reduces the possibility of problems that result from out-of-date information.
Training as a Key Expense
- Significant Investment – Training and onboarding expenses, including initial training, workflow adjustments, and ongoing education, are a significant part of how much does Epic cost for a hospital.
- Ensuring System Efficiency – Without proper training, hospitals may face inefficiencies and errors, which could diminish the return on investment in Epic. Hospitals must thus give priority to this element in order to take full advantage of the platform’s potential.
Customization Fees: Tailoring the System to Fit Hospital-Specific Needs
Epic Systems offers extensive customization options to align with the unique needs of each hospital, but this flexibility comes at a cost. Customization can be one of the largest expenses in the overall implementation process. When calculating how much does Epic cost for a hospital, customization fees are a key component that can significantly impact the total investment.
Custom Workflow Design
- Hospital-Specific Processes – Every hospital operates with different workflows related to patient data management, billing, and inter-departmental coordination. Hospitals can customize these workflows with Epic to align with their own procedures, guaranteeing a smooth transition.
- Cost of Customization – Customizing workflows requires Epic-certified developers and consultants, and the fees can range from $100,000 to several million dollars, depending on the complexity and extent of customization. Hospitals requiring major modifications to fit their operational needs will see how much does Epic cost for a hospital increase proportionally due to these services.
Specialty Modules
- Department-Specific Features – Epic offers specialized modules for various medical disciplines such as oncology, cardiology, and pediatrics, allowing hospitals to optimize care for specific patient populations.
- Additional Licensing and Setup – Each module requires separate licensing and setup fees, which can drive costs into the six or seven-figure range, depending on the number of departments requiring customization. As a result, hospitals need to carefully evaluate how many specialized modules are necessary when considering how much does Epic costs for a hospital.
Integrating Third-Party Systems
- Third-Party System Compatibility – Many hospitals rely on third-party systems for specific functions such as laboratory management, radiology, or billing. To enable smooth data sharing between platforms, bespoke work is needed for the integration of these systems with Epic.
- Integration Fees – Integration costs can vary from $50,000 to over $500,000, depending on the complexity of the third-party systems. Hospitals that rely heavily on external systems need to account for these costs when assessing how much does Epic cost for a hospital.
Impact of Customization on Overall Costs
- Customization Adds Flexibility – Customizing Epic to fit a hospital’s needs ensures that the system aligns with existing workflows, enhances department-specific care, and integrates with other tools, ultimately increasing operational efficiency.
- Customization Costs Vary Widely – However, these benefits come with substantial fees, and hospitals must carefully factor them into their overall budget. The size, complexity, and scope of the hospital’s operations will influence the final cost, and understanding how much does Epic cost for a hospital with customization is essential for accurate financial planning.
Personalization as a Major Cost Factor
Customization is a powerful feature of Epic Systems which enables hospitals to tailor the platform to meet specific clinical and operational needs. However, these adjustments can add significantly to the initial implementation costs. Hospitals must consider customization fees, alongside other factors like licensing, hardware, and training, to fully grasp how much does Epic cost for a hospital and plan their budgets accordingly. Customization facilitates long-term improvements in patient care and operational efficiency which makes it a worthwhile investment for many institutions.
4. Hidden and Ongoing Costs of Epic Implementation
While hospitals often focus on the initial costs of implementing Epic Systems, it’s equally important to consider the hidden and ongoing expenses that can arise throughout the life of the system. Understanding these costs is crucial when assessing how much does Epic cost for a hospital in the long run. Below are some of the key ongoing expenses that hospitals must account for:
Maintenance and Support Fees: Keeping the System Running Smoothly Over Time
Once Epic Systems is implemented, hospitals need to account for ongoing maintenance and support costs to ensure the platform operates efficiently and securely over time. It is essential for a system to keep itself updated to regulate the overall budget. When assessing how much does Epic cost for a hospital, understanding these recurring fees is essential.
Annual Maintenance Fees
- Recurring Costs – Epic typically charges annual maintenance fees that range from 15% to 20% of the total software licensing costs. These charges take care of regular software maintenance or checkup, upgrades and bug repairs.
- Cost Example – For a hospital that has invested $1 million in licensing, the annual maintenance fees could amount to between $150,000 and $200,000. This cost is often overlooked when hospitals consider how much does Epic cost for a hospital, yet it represents a significant long-term expense that must be factored into the overall budget.
Technical Support
- Need for Assistance – Hospitals may require ongoing technical support to troubleshoot issues or assist with system modification and is important for organizations without robust internal IT teams.
- Variable Costs – The costs for technical support services can vary widely based on the level of service required and the complexity of the issues faced. For example, hospitals may need to pay several thousand dollars annually for these services, particularly if they face frequent technical challenges. Understanding these support costs is crucial for accurately estimating how much does Epic cost for a hospital over the long term.
System Monitoring and Upkeep
- Ensuring Optimal Performance – To maintain optimal system performance, hospitals may need to invest in system monitoring tools and services.
- Budget Considerations – The costs associated with these monitoring tools can vary, but they should be included in the overall budget for maintenance and support. Hospitals should remain aware of these additional expenses when evaluating how much does Epic cost for a hospital.
Comprehensive Cost Considerations
Ongoing maintenance and support fees are vital to the long-term success of Epic Systems in a hospital setting. By accounting for annual maintenance fees, technical support, and system monitoring costs, hospitals can develop a more accurate understanding of how much does Epic cost for a hospital over time.
System Upgrades: Regular Updates to Stay Compliant with Healthcare Regulations
In the ever-evolving landscape of healthcare, hospitals must ensure their Electronic Health Record (EHR) systems, like Epic, remain compliant with new regulations and security standards. This necessitates regular system upgrades, which come with their own costs. It is important to understand these expenses or costs for hospitals or healthcare providers when evaluating how much does Epic cost for a hospital.
Scheduled Upgrades
- Periodic Releases – Epic periodically rolls out new versions of its software, which include essential updates, feature enhancements, and performance improvements.
- Budgeting for Upgrades – Hospitals typically need to allocate funds for these upgrades, which can range from $100,000 to $500,000, depending on the complexity of the updates and the size of the hospital.
- Additional Training Costs – Some upgrades may require staff retraining or adjustments to existing workflows, adding to the overall expenses. These ongoing upgrade costs are critical to consider when determining how much does Epic cost for a hospital, as they can accumulate significantly over time.
Compliance Costs
- Staying Compliant – To maintain compliance with healthcare regulations such as HIPAA and the 21st Century Cures Act, hospitals may need to implement additional modifications or enhancements to their EHR systems.
- Financial Implications – Compliance-related upgrades can incur substantial costs, which should be factored into the hospital’s budget for ongoing expenses. It’s essential for hospitals to proactively assess how much does Epic cost for a hospital in light of these regulatory changes to avoid unexpected expenses.
Data Security Enhancements
- Adapting to Cyber Threats – With the increasing sophistication of cyber threats, Epic must continually update its security measures to protect sensitive patient data.
- Cost of Security Measures – Hospitals may incur costs related to these data security enhancements, which can include both software and hardware upgrades.
- Long-Term Financial Planning – It is essential for hospitals to incorporate these security-related costs when evaluating how much does Epic cost for a hospital over the long run.
Potential Downtime Costs: Financial Impact During Installation and Transition Periods
When hospitals implement Epic Systems, one critical aspect often overlooked is the potential downtime costs that can occur during the transition from legacy systems to the new Electronic Health Record (EHR) platform. It is important to understand these costs to evaluate how much does Epic cost for a hospital.
Disruption to Operations
- Temporary Operational Disruptions – The transition to Epic can lead to significant disruptions as staff members familiarize themselves with the new system and workflows are modified.
- Impact on Revenue – Disruptions can result in delays in patient processing and care delivery, leading to potential lost revenue. Hospitals need to consider these operational disruption costs when calculating how much does Epic cost for a hospital.
Impact on Patient Care
- Patient Experience – Downtime can adversely affect patient care, resulting in increased wait times and decreased patient satisfaction. Delays or inefficiencies in patient care can cause unhappiness which can damage the hospital’s reputation.
- Long-Term Effects – Reputational damage from poor patient experiences during the transition can have lasting financial implications. Evaluating how much does Epic cost for a hospital must include these potential impacts on patient care and satisfaction during the critical transition period.
Temporary Staffing Costs
- Need for Additional Staffing – To maintain patient care standards during the transition, hospitals may need to hire temporary staff or offer overtime to existing employees. This can lead to additional staffing costs that can accumulate quickly.
- Budgeting for Transition Expenses – These temporary staffing costs should be included in the total implementation expenses. Understanding how much does Epic cost for a hospital requires factoring in these potential additional costs that arise during the transition period.
5. How Hospital Size Affects Epic Pricing
The size and complexity of a hospital significantly influence the overall costs associated with implementing Epic Systems. Understanding how hospital size affects pricing is essential for administrators considering how much does Epic cost for a hospital.
Small Hospitals vs. Large Health Systems: How Scale Influences Cost
Cost Structures
- Negotiating Power – Larger health systems often have the leverage to negotiate better pricing terms with Epic due to their scale. They can secure discounts on software licenses, training, and ongoing support, leading to lower costs per bed or per patient.
- Higher Rates for Small Hospitals – Conversely, small hospitals, with limited budgets and fewer patients, tend to pay higher rates relative to their size. This pricing disparity means that the answer to how much does Epic cost for a hospital can vary dramatically based on the institution’s size.
Implementation Complexity
- Complexity in Large Systems – Large health systems typically require more complex implementations, encompassing multiple departments, specialties, and facilities. This complexity results in higher initial costs for software, hardware, and training for the healthcare facilities.
- Simpler Processes for Small Hospitals – Small hospitals generally face a simpler implementation process, which can lower their overall costs. However, the initial lower expenses can be misleading if they overlook ongoing costs related to training and maintenance.
Operational Needs
- Advanced Features for Large Systems – Larger health systems may require more advanced features and modules to meet their diverse operational needs such as oncology, pediatrics, or cardiology, which can increase overall costs.
- Essential Functionalities for Smaller Hospitals – In contrast, smaller hospitals might focus on essential functionalities, leading to lower overall expenses. Therefore, the specific needs of each hospital, driven by its size and complexity, have a direct impact on how much does Epic cost for a hospital.
6. The Epic Systems Total Cost of Ownership (TCO)
Understanding the Total Cost of Ownership (TCO), which includes both the original investment and any recurring expenses as well as potential long-term financial advantages, is crucial when assessing Epic Systems. This comprehensive view enables hospitals to assess how much does Epic cost for a hospital in both the short and long term.
Direct vs. Indirect Costs: Beyond the Initial Investment
Direct Costs
Direct costs refer to the tangible expenses associated with the implementation of Epic, including:
- Software Licensing – The initial fees for acquiring Epic software, which can range significantly based on hospital size and chosen modules.
- Hardware and Infrastructure – Costs related to purchasing and upgrading servers, workstations, and network equipment necessary to support Epic.
- Training and Onboarding – Expenses incurred for staff training, which are crucial for successful implementation and usage.
For hospitals evaluating how much does Epic cost for a hospital, these direct costs are often the most visible and straightforward to calculate. However, they represent only part of the overall TCO.
Indirect Costs
Indirect costs can significantly impact the TCO but may be more challenging to quantify. Among them are:
- Disruptions to Operations – The potential loss of productivity during the transition to the new system can affect patient care and operational efficiency. Hospitals may experience longer wait times or reduced staff availability which leads to decreased patient satisfaction and potential revenue loss.
- Ongoing Maintenance and Support – While hospitals anticipate maintenance fees, the costs associated with ongoing technical support, upgrades, and training must also be factored in as indirect expenses.
- Change Management – The time and resources spent on managing organizational change during the implementation of Epic can incur costs related to temporary staffing, project management, and additional training.
6. Return on Investment (ROI) Considerations: Financial Benefits Over Time
Improved Efficiency
- Streamlined Workflows – Implementing Epic Systems can lead to significant improvements in operational efficiency. Epic’s comprehensive EHR platform regulates workflows which reduces redundant data entry.
- Boost Communication – The system improves communication among healthcare teams which saves time and resources.
- Impact on ROI – These efficiency gains contribute to the overall ROI and must be considered when evaluating how much does Epic cost for a hospital.
Enhanced Patient Care
- Quality of Care – Epic’s EHR platform enhances patient care quality through improved data accessibility and accuracy.
- Informed Decision-Making – Real-time access to patient information allows healthcare providers to make informed decisions quickly, leading to better health outcomes.
- Attracting Patients – Improved patient outcomes can potentially reduce the length of hospital stays, enhance hospital reputations, and attract more patients, thus increasing revenue.
- Calculating Costs – These long-term benefits play a crucial role in calculating ROI and understanding how much does Epic cost for a hospital.
Regulatory Compliance and Risk Mitigation
- Maintaining Compliance – Epic Systems assists hospitals in maintaining compliance with healthcare regulations, which reduces the risk of costly penalties.
- Data Security – The system’s strong data security features minimize the risk of data breaches, which can have significant financial consequences.
- Cost Savings – By accounting for the cost savings associated with compliance and risk mitigation, hospitals can better understand the ROI of their investment in Epic and how it affects how much does Epic cost for a hospital.
Long-Term Cost Savings
- Upfront vs. Long-Term Costs – Although the upfront costs of Epic may be substantial, hospitals can realize long-term cost savings that improve ROI.
- Cumulative Benefits – Over time, operational efficiencies, improved patient care, and reduced compliance risks contribute to significant financial benefits.
- Financial Analysis – Hospitals should analyze projected cost savings against the initial investment to assess how much does Epic cost for a hospital over the long term.
Key Takeaways
- Financial Benefits Beyond Initial Costs – The financial benefits of implementing Epic Systems extend beyond initial costs.
- Important Evaluation Elements – Hospitals can evaluate the ROI of their investment effectively by focusing on improved efficiency, enhanced patient care, compliance, and long-term savings.
- Crucial for Administrators – Ultimately, understanding all these factors is crucial for hospital administrators when considering how much does Epic cost for a hospital.
The Long-Term Value of Epic: Why Some Hospitals Justify the High Upfront Cost
Comprehensive Features and Functionality
- Extensive Range of Features – Epic is renowned for its comprehensive features and functionalities, making it one of the leading EHR systems available.
- All-in-One Approach – Hospitals that invest in Epic gain access to robust modules covering various healthcare management aspects, from scheduling to billing and clinical documentation.
- Simplifying Operations – This integrated approach simplifies operations and improves coordination which helps justify the higher initial investment by enhancing overall efficiency.
Compatibility and Integration
- Commitment to Cooperation – Epic emphasizes interoperability, allowing seamless integration with other healthcare systems and data exchange.
- Value-Based Care Initiatives – This capability is crucial for hospitals looking to participate in value-based care initiatives and collaborative healthcare networks.
- Strategic Positioning – By investing in a system that enhances collaboration, hospitals can strategically position themselves within the healthcare ecosystem, making the upfront costs more palatable in light of potential long-term benefits.
Scalability for Future Growth
- Adaptable Technology Needs – As hospitals grow and evolve, their healthcare technology requirements change.
- Modular Design – Epic’s modular design allows institutions to scale their systems as needed, adding new functionalities and modules as they expand services.
- Cost-Effective Future-Proofing – This scalability means hospitals won’t need to switch EHR systems in the future, which can be both costly and disruptive. Understanding how much does Epic cost for a hospital should include this long-term adaptability and future-proofing aspect.
Long-Term Partnerships
- Ongoing Support and Training – Many hospitals view their relationship with Epic as a long-term partnership rather than a one-time transaction.
- Maximizing Investment – Epic provides ongoing support, training, and updates that help hospitals maximize their investment over time.
- Greater Long-Term Benefits – This partnership can lead to substantial benefits over time, making the initial costs more justifiable.
Key Takeaways
- Total Cost of Ownership (TCO) – The Total Cost of Ownership (TCO) for Epic Systems encompasses both direct and indirect costs as well as potential long-term financial benefits.
- Critical ROI Considerations – Understanding the ROI considerations and the long-term value of Epic is crucial for hospitals evaluating how much does Epic cost for a hospital.
- Informed Decision-Making – Hospital administrators can make informed decisions that align with their strategic goals which ensure a positive impact on patient care and operational efficiency over time.
7. Financing Epic: Payment Options and Strategies
Financing the implementation of Epic Systems is crucial for hospitals as they assess how much does Epic cost for a hospital. Given the substantial initial investment required, understanding various payment options and financing strategies can help healthcare institutions make informed decisions.
Purchasing Models: Leasing, Purchasing, and Subscription-Based Pricing
Leasing Options
- Flexible Access – Leasing provides hospitals with a flexible way to access Epic’s EHR system without a significant upfront capital investment.
- Payment Structure: Under a leasing agreement, hospitals pay monthly or quarterly fees to use the software and hardware.
- Cash Flow Management – This option is particularly appealing for smaller hospitals or those with tight budgets, as it allows for better cash flow management.
- Long-Term Costs – It is essential to calculate the total cost of leasing over time, as it may end up being more expensive than a one-time purchase. Evaluating leasing against the question of how much does Epic cost for a hospital can provide insights into long-term financial commitments.
Purchasing Upfront
- Significant Initial Investment – Some hospitals may opt to purchase Epic outright, requiring a substantial upfront payment.
- Long-Term Financial Advantages – This option can be financially advantageous in the long term, as hospitals own the system outright and avoid ongoing leasing costs.
- Initial Financial Burden – However, the initial financial burden can be daunting, especially for smaller institutions. When determining how much does Epic cost for a hospital, it’s essential to weigh both the immediate financial impact and the long-term benefits of ownership.
Subscription-Based Pricing
- Recurring Fees – Epic offers subscription-based pricing models, allowing hospitals to pay a recurring fee for access to the software.
- Predictable Budgeting – This model is beneficial for hospitals that prefer predictable budgeting and want to avoid large upfront costs.
- Inclusion of Updates and Support – Subscription fees typically include software updates and ongoing support, simplifying budgeting for ongoing expenses.
- Long-Term Cost Analysis – However, hospitals must analyze the long-term costs of this model to understand how it affects their overall investment and operational strategy concerning how much Epic cost for a hospital.
Government Incentives and Grants: Leveraging Funding Opportunities Like HITECH
When evaluating how much does Epic cost for a hospital, understanding the available government incentives and grants can significantly impact the overall investment. Hospitals can take advantage of a number of financial options to assist defray the costs of putting Epic Systems into practice.
HITECH Act Incentives
- Financial Incentives for EHR Adoption – The Health Information Technology for Economic and Clinical Health (HITECH) Act offers financial incentives to hospitals that adopt and effectively use EHR systems like Epic.
- Meaningful Use Reimbursements – Hospitals can receive reimbursement payments for demonstrating meaningful use of EHR technology. This funding can significantly reduce the costs associated with implementing Epic which makes it essential for administrators to explore these incentives when assessing how much does Epic cost for a hospital.
State and Local Grants
- Funding Opportunities for Technology Investments – Various state and local governments provide grants and funding opportunities to support healthcare organizations in their technology investments.
- Improving Healthcare Access and Patient Care – These grants may focus on improving healthcare access, enhancing patient care, or advancing public health initiatives. Hospitals should actively research available funding opportunities within their regions to supplement the costs associated with Epic.
- Alleviating Financial Burdens – Utilizing state and local grants can alleviate some of the financial burdens of adopting Epic Systems, enhancing the overall investment and making it more manageable when evaluating how much does Epic cost for a hospital.
Tax Incentives
- Tax Deductions and Credits – In addition to direct funding, some hospitals may benefit from tax incentives related to their investment in health IT that reduce their overall tax liability by implementing advanced EHR systems.
- Minimizing Expenditures – Understanding the full scope of potential financial incentives is crucial for hospitals seeking to minimize expenditures while investing in Epic. This knowledge is particularly important when analyzing how much does Epic cost for a hospital.
Collaborative Financing: Sharing the Cost in a Multi-Hospital System
Implementing Epic Systems can be a significant financial undertaking for hospitals. A health system or network’s numerous hospitals can strategically split the investment’s costs by utilizing collaborative finance. Understanding how collaborative financing impacts how much does Epic cost for a hospital can led to more effective financial planning and improved access to essential EHR capabilities.
Multi-Hospital Collaborations
- Pooling Resources – Hospitals that are part of a health system can collaborate to pool their resources, reducing individual financial burdens. Better negotiating strength with Epic is made possible by this joint strategy, which frequently results in cheaper software.
- Cost Reduction Benefits – By sharing the costs of implementation, hospitals can alleviate the financial pressure on each facility, making it easier to budget for Epic. This guides healthcare providers on how much does Epic cost for a hospital.
Shared Services Models
- Joint Investment Infrastructure – Hospitals can explore shared services models, where they collectively invest in the infrastructure and support services necessary for Epic implementation including IT personnel, training programs, and maintenance agreements.
- Economies of Scale – Hospitals can achieve economies of scale which lead to lower overall costs and can greatly impact the total investment in Epic. This guides that using cooperative finance methods assess how much does Epic cost for a hospital.
Joint Purchasing Agreements
- Negotiating Power Through Collaboration – Establishing joint purchasing agreements allows hospitals to collaborate and purchase Epic as a group. This collaborative buying power can lead to better pricing and terms which ultimately reduces the financial impact on individual facilities.
- Benefits for Smaller Hospitals – Joint purchasing agreements are particularly beneficial for smaller hospitals, which may lack the leverage to negotiate favorable terms on their own. These hospitals can enhance their bargaining power which significantly affects how much does Epic cost for a hospital.
8. Comparing Epic to Competitors
When evaluating how much does Epic cost for a hospital, it’s essential to compare it with its primary competitors, such as Cerner and Allscripts. Every electronic health record system has advantages and disadvantages pertaining to cost, functionality, and total worth.
Epic vs. Cerner: Which is More Cost-Effective?
Pricing Models
- Epic – Epic’s pricing typically involves substantial upfront costs, including software licenses, hardware, and training expenses. Hospitals may also choose subscription-based models which could result in recurring costs that are predictable.
- Cerner – Cerner often offers competitive pricing, especially for smaller hospitals. By allowing institutions to choose only the capabilities they require, their modular pricing structure may help reduce upfront expenses. For example, a smaller hospital may pay less for a basic EHR solution from Cerner compared to Epic’s comprehensive offerings.
Cost-Effectiveness
- Hospitals must weigh the total costs, including initial investment and ongoing expenses, when determining which system is more cost-effective. For larger health organizations, Epic’s vast capabilities and long-term support might justify the investment despite its higher initial price. On the other hand, because of its reduced starting cost, Cerner might be more enticing to smaller facilities, making it a better choice for businesses with tight budgets.
Implementation and Support Costs
- Both Epic and Cerner require investment in training and support. Hospitals do, however, frequently note that Epic’s training programs are longer, which could result in increased upfront expenses. On the other hand, Cerner may offer more affordable ongoing support, impacting the overall financial comparison. When assessing how much does Epic cost for a hospital, it is vital to factor in these implementation and support costs alongside licensing fees.
Epic vs. Allscripts: Feature Comparison and Pricing Models
Feature Set
- Epic – Known for its comprehensive and robust feature set, Epic offers modules for everything from electronic health records to billing, patient engagement, and population health management. One of its main advantages is its collaboration or cooperation to facilitate information sharing between healthcare providers and patients.
- Allscripts – Allscripts provides a more flexible and modular approach that allows hospitals to customize their EHR based on specific requirements. Despite its strong clinical features and widespread reputation for usability, Allscripts could not have all of Epic’s sophisticated features.
Pricing Models:
- Epic – Epic typically involves higher upfront costs for its full suite of functionalities, along with ongoing maintenance fees. However, hospitals can negotiate pricing based on size and specific needs.
- Allscripts – Allscripts often appeals to smaller and mid-sized hospitals due to its competitive pricing and modular options. Hospitals can choose to implement only the functionalities they require, which can significantly lower the initial investment. This flexibility is crucial when analyzing how much does Epic cost for a hospital compared to Allscripts.
Return on Investment:
- Whereas Epic may provide extensive features that support comprehensive patient care, Allscripts may be a more affordable option for hospitals with simpler requirements. Hospitals must evaluate their specific requirements and long-term goals when considering how much does Epic cost for a hospital in comparison to Allscripts.
Is Epic the Right Choice for All Hospitals? Weighing Cost Versus Capability
Evaluating Hospital Needs
- Not all hospitals require the extensive capabilities offered by Epic. Smaller facilities or those with limited resources may find that the high upfront costs and comprehensive features do not align with their operational needs. Conversely, larger health systems with complex requirements may justify the investment in Epic for its robust functionalities and long-term support.
Budget Considerations
- Hospitals must consider their budgets when determining if Epic is the right choice. The comprehensive features and significant upfront expenses may not meet the operational needs of smaller establishments or those with limited resources. Whereas, larger institutions might find that the investment in Epic’s advanced capabilities which lead to boost operational efficiencies and patient care.
Long-Term Strategic Goals
- Ultimately, the decision to choose Epic should align with a hospital’s long-term strategic goals. Even while there could be greater upfront expenses, there may be long-term benefits in the form of increased patient care, increased efficiency, and partnerships with Epic. Hospitals must evaluate how much does Epic cost for a hospital against these strategic priorities to determine if the investment is worthwhile.
Scalability and Future Growth
- Hospitals anticipating future growth and the need for advanced features may find that Epic offers a scalable solution that can evolve with their needs. In contrast, smaller or rural hospitals that do not anticipate significant expansion may find greater value in more affordable options like Cerner or Allscripts.
9. Trends and Forecasts for EHR Pricing in the Future
The environment of electronic health records (EHRs) is changing quickly, and with it, the cost of EHRs in the future. It is important for hospitals to understand these trends to evaluate how much does Epic cost for a hospital and the broader implications for EHR investments.
Evolving EHR Technology: How Advancements May Drive Costs Up or Down
Innovation and Functionality Expansion
- Continuous Technological Growth – As EHR systems like Epic evolve, vendors invest in research and development to introduce advanced features such as telehealth capabilities, patient engagement tools, and robust data analytics.
- Impact on Licensing Fees – These new functionalities can lead to increased licensing fees as hospitals adopt innovative solutions, adding to how much does Epic cost for a hospital.
- Price Hikes with New Features – Hospitals must be prepared for potential price hikes when new tools become part of the standard offering, influencing how much does Epic cost for a hospital over time.
Enhanced Cooperation Standards
- Seamless Data Exchange – As the demand for interoperable systems grows, EHR providers like Epic are focusing on integrating features that facilitate seamless data sharing among different healthcare platforms.
- Short-Term Cost Increase – Initially, incorporating these collaborative features may increase how much does Epic cost for a hospital due to necessary system updates.
- Long-Term Savings Potential – However, in the long term, hospitals can benefit from better care coordination and reduced duplication of services, which ultimately reduces how much does Epic cost for a hospital over time.
Regulatory Compliance
- Adapting to Regulatory Changes – As regulations in the healthcare industry continue to evolve, EHR vendors are required to update their systems to meet new compliance standards.
- Upgrades and Compliance Costs – These ongoing updates can temporarily raise how much does Epic cost for a hospital, especially as compliance requirements change.
- Mitigating Financial Risks – By staying compliant with industry regulations, hospitals reduce the risk of penalties and fines, which can offset how much does Epic cost for a hospital in the long term.
Assessing the Total Cost of Ownership (TCO)
- Balancing Innovation and Costs – As Epic introduces new innovations, hospitals need to balance the initial cost of adoption with the long-term benefits, including operational efficiency and patient outcomes. This affects how much does Epic cost for a hospital overall.
- Budgeting for Upgrades – Hospitals should consider how regular system updates, driven by regulatory changes and technology advancements, impact how much does Epic cost for a hospital on an annual basis.
Cloud-Based Solutions and Cost: How SaaS Models Are Changing the Pricing Landscape
Shift to Cloud-Based EHRs
- Growing Trend – Many healthcare organizations are moving toward cloud-based EHR solutions, which offer greater flexibility and scalability compared to traditional on-premises systems.
- Lower Upfront Costs – Cloud-based systems generally have lower initial costs, reducing the financial strain on hospitals. This shift can impact how much does Epic cost for a hospital, as upfront investments in hardware and infrastructure are minimized.
- Scalability and Flexibility – Cloud solutions allow hospitals to scale their services easily, adjusting usage based on demand, which also affects how much does Epic cost for a hospital as services expand.
Subscription Pricing Models
- SaaS Subscription – With Software-as-a-Service (SaaS) models, hospitals pay for EHR access on a recurring subscription basis, instead of making large upfront purchases.
- Improved Budgeting – Subscription pricing makes it easier for hospitals to predict and manage their budgeting needs. Hospitals can spread costs over time, leading to more predictable expenses when assessing how much does Epic cost for a hospital.
- Long-Term Costs – While subscription models often lower initial expenses, hospitals should evaluate long-term costs and potential future price increases to fully understand how much does Epic cost for a hospital over time.
Cost of Cloud Migration
- Data Migration Costs – Moving to a cloud-based EHR system requires a thorough data migration process, which can incur significant costs depending on the hospital’s size and data volume.
- Training and Integration – Hospitals also need to factor in training for staff and integration with existing systems, which can add to the overall cost of adopting cloud-based Epic solutions. These costs will impact how much does Epic cost for a hospital in both the short and long term.
- Balancing Short- and Long-Term Expenses – Although the initial transition may be costly, hospitals need to assess potential long-term savings, such as reduced IT maintenance and enhanced system flexibility, when calculating how much does Epic cost for a hospital.
The Impact of AI and Machine Learning on EHR Pricing: New Costs and Opportunities
AI-Driven Features and Automation
- Enhanced Capabilities – As AI and machine learning become more integrated into EHR systems like Epic, they bring improvements such as automation of routine tasks, smarter workflows, and better patient outcomes.
- Increased Initial Costs – The integration of these advanced technologies can lead to higher initial investments. When evaluating how much does Epic cost for a hospital, it is important to consider the costs of implementing AI-powered features and the potential need for specialized hardware or software upgrades.
Operational Savings through AI
- Automation Benefits – AI can automate repetitive administrative and clinical tasks, such as data entry, billing, and scheduling which reduces the workload for healthcare staff and labor cost savings in the long run.
- Improved Decision-Making – AI-enhanced systems can provide predictive analytics and decision support, helping clinicians make more informed and timely choices.
- Long-Term ROI – While AI may increase initial costs, the operational savings and efficiencies gained can more than compensate for these expenses. Hospitals should weigh these long-term benefits when calculating how much does Epic cost for a hospital.
Data-Driven Insights and Value-Based Care
- Advanced Analytics – AI and machine learning enable hospitals to leverage vast amounts of data for deeper insights into patient care. Healthcare professionals are assisted or guided in making more accurate clinical judgments for improved patient outcomes by means of this data-driven technique or approach.
- Value-Based Care Models – As healthcare moves toward value-based care, which rewards quality over quantity, AI can play a critical role. AI’s predictive powers help hospitals better manage chronic illnesses and make better use of their resources in the healthcare facility.
- Impact on Pricing – Hospitals adopting AI-powered EHR systems need to consider how these advancements can affect both short-term investments and long-term savings when determining how much does Epic cost for a hospital.
10. Decisions of Strategic Investment in Epic Systems
Investing in an electronic health record (EHR) system is a significant decision for any hospital, particularly when considering how much does Epic cost for a hospital.
Cost-Benefit Analysis: Balancing Short-Term Costs with Long-Term Gains
Understanding Upfront and Ongoing Costs
- Upfront Costs – When implementing Epic, hospitals face significant initial investments, including software licensing, hardware procurement, and extensive training programs for staff. These upfront costs often play a critical role in determining how much does Epic cost for a hospital.
- Ongoing Costs – Beyond the initial implementation, hospitals must account for ongoing expenses such as system maintenance, software support, updates, and potential future upgrades. These recurring costs need to be included in the overall financial evaluation.
Evaluating Long-Term Benefits
- Improved Patient Care – Epic’s comprehensive EHR system enhances patient care by providing real-time access to medical records and improving care coordination across departments.
- Operational Efficiency – pic automates various administrative tasks, reducing manual workload and increasing staff productivity, which can lead to significant operational savings over time.
- Reduced Errors – The system minimizes errors related to patient data and billing, leading to more accurate clinical decisions and financial transactions.
- Revenue Growth: With streamlined billing and coding processes, hospitals can see improved revenue collection. Factoring these long-term gains is essential when estimating how much does Epic cost for a hospital.
Quantifying Intangible Benefits
- Patient Satisfaction – The improved efficiency and accuracy of Epic’s system often result in higher patient satisfaction, as patients experience shorter wait times and more personalized care.
- Staff Morale – Streamlining workflows and reducing redundant tasks can lead to higher job satisfaction among staff, improving overall morale.
- Regulatory Compliance – Epic helps hospitals remain compliant with healthcare regulations, reducing the risk of costly fines. Estimating the value of these intangible benefits is important when considering how much does Epic cost for a hospital.
Scenario Planning
- Best-Case Scenario – This scenario might involve lower-than-expected implementation costs, higher patient volume, and greater operational efficiencies, resulting in faster ROI.
- Worst-Case Scenario – This could include higher implementation and training costs, slower patient volume growth, and extended timelines to achieve expected savings.
- Most-Likely Scenario – Typically, hospitals will balance both optimistic and conservative estimates, helping them determine the true potential for ROI. It is important for hospitals to understand scenario planning related to how much does Epic cost for a hospital and making informed investment decisions.
Steps to Evaluate EHR Systems: What Hospitals Should Consider Before Purchasing
Identify Key Requirements
- Define Essential Features – Hospitals must begin by identifying their specific needs, including harmonized reporting capabilities, patient engagement tools, and mobile access. Hospitals can compare different EHR systems with confidence provided they have a comprehensive understanding of the key features.
- Customization Needs – Hospitals should also consider how much customization they need and how that will impact their decision-making, especially in determining how much does Epic cost for a hospital compared to competitors.
Conduct Market Research
- Vendor Research – Conduct thorough market research to explore leading EHR systems such as Epic, Cerner, and Allscripts and Hospitals can learn about other companies with these systems.
- Competitive Comparison – Understanding the pros and cons of different EHR systems allows hospitals to make informed comparisons regarding pricing and functionality, key aspects of understanding how much does Epic cost for a hospital.
Request Demos and Trials
- Hands-On Experience – Engaging vendors for demonstrations or trial periods provides direct experience with the EHR system’s interface and usability.
- Cost-Benefit Analysis – Trials help hospitals assess potential cost savings versus upfront and ongoing expenses, aiding in the comprehensive evaluation of how much does Epic cost for a hospital versus other options.
Engage Stakeholders
- Multidisciplinary Input – It is important to involve key stakeholders from clinical, administrative, and IT departments to get a holistic view of the hospital’s requirements.
- Ensuring Alignment – By gathering input from multiple departments, hospitals can ensure that the chosen EHR system addresses organizational needs while also providing value relative to how much does Epic cost for a hospital.
Evaluate Vendor Support and Training
- Support Services – Understanding the level of ongoing support offered by vendors, including Epic, is vital for long-term system success. Hospitals should ask about service level agreements (SLAs), support hours, and response times.
- Training Programs – Effective training programs are critical to smooth implementation. Hospitals must consider the costs of training and how this contributes to their overall understanding of how much does Epic cost for a hospital.
Analyze Integration Capabilities
- System Compatibility – Evaluate how easily a new EHR system integrates with existing hospital software, such as billing, scheduling, and lab systems.
- Additional Costs – Hospitals should consider whether poor integration may lead to additional expenses, further influencing how much does Epic cost for a hospital during implementation and beyond.
Expert Advice for Hospital Executives: Tips from CIOs Who Have Implemented Epic
Prioritize Change Management
- Engage Early – CIOs highlight the importance of engaging staff at all levels early in the process to reduce resistance and increase adoption.
- Ongoing Support – Continuous support during and after the transition helps mitigate challenges, which is crucial when understanding how much does Epic cost for a hospital in terms of both financial and human resources.
Focus on Data Governance
- Data Quality and Security – Implement clear data governance policies to ensure data integrity and compliance with regulations for effective EHR operation for healthcare facilities.
- Integration with Existing Systems – Effective data governance will ensure smooth integration with existing workflows, influencing how much does Epic cost for a hospital in the long term.
Budget for Contingencies
- Plan for the Unexpected – Unexpected costs are common during EHR implementation. CIOs advise allocating extra funds for contingencies, covering unexpected training needs, system upgrades, or custom enhancements.
- Managing Overruns – Contingency budgeting helps ensure that hospitals remain prepared for unforeseen costs when evaluating how much does Epic cost for a hospital during the implementation phase.
Learn from Peers
- Industry Networking – Learning from other hospital leaders who have implemented Epic is invaluable and participate in industry conferences and peer-to-peer discussions to gather insights and information.
- Sharing Successes and Challenges – By learning from others’ successes and challenges, executives can better estimate how much does Epic cost for a hospital and avoid common pitfalls.
Measure Success
- Define Metrics – Establish clear success metrics such as patient satisfaction, operational efficiency, and financial performance. CIOs stress that these should be tracked over time to assess return on investment (ROI).
- Continuous Improvement – Regularly reviewing these performance metrics will help hospitals refine their strategies and make informed decisions about how much does Epic cost for a hospital in terms of ongoing value and benefits.
11. Challenges to Epic Implementation in Hospitals and Their Remedies
Resistance to Change
- Nature of the Challenge – Resistance to adopting new technologies is common, as staff may fear disruption to their workflow or the complexity of learning a new system.
- Potential Solutions:
- Involve Key Stakeholders – Engaging clinicians and administrative staff in the decision-making process helps foster support. Explaining how much does Epic cost for a hospital allows staff to see the value of the investment.
- Implement Change Management Strategies – Structured change management with ongoing communication ensures staff understand the benefits of Epic and the importance of the transition.
Data Migration Issues
- Nature of the Challenge – Migrating data from legacy systems to Epic can lead to data loss or corruption.
- Potential Solutions:
- Conduct Thorough Data Audits – Performing detailed audits before migration helps identify discrepancies. Understanding how much does Epic cost for a hospital helps allocate resources for data checks.
- Utilize Expert Consultants – Experienced consultants can facilitate smoother data migration, reducing risks and ensuring data accuracy, which is essential given how much does Epic cost for a hospital.
Integration with Existing Systems
- Nature of the Challenge – Integrating Epic with existing hospital systems like billing and lab systems can be complex.
- Potential Solutions:
- Engage IT Teams Early – Early collaboration with IT helps assess integration needs and clarify how much does Epic cost for a hospital in terms of integration efforts.
- Choose Modular Implementations – Implementing Epic’s features gradually help manage costs and reduce integration challenges, impacting how much does Epic cost for a hospital.
Training and Onboarding Challenges
- Nature of the Challenge – Staff with diverse learning styles and varying tech skills can face difficulties in training.
- Potential Solutions:
- Create Tailored Training Programs – Custom training for clinical and administrative staff ensures effective learning and maximizes the return on investment, reflecting on how much does Epic cost for a hospital.
- Offer Continuous Support – Ongoing support after training helps staff become comfortable with the system and contributes to a better understanding of how much does Epic cost for a hospital in terms of resource allocation.
Project Management and Timeline Delays
- Nature of the Challenge – Implementation delays can increase costs and disrupt hospital operations.
- Potential Solutions:
- Establish Clear Timelines – Setting realistic timelines with buffer periods helps manage expectations. Proper planning ensures hospitals understand how much does Epic cost for a hospital during delays.
- Utilize Experienced Project Managers – Engaging specialized project managers helps streamline implementation, reducing delays and controlling how much does Epic cost for a hospital.
Budget Overruns
- Nature of the Challenge – Costs can exceed projections due to unforeseen factors, complicating financial planning.
- Potential Solutions:
- Develop a Comprehensive Budget – Creating a detailed budget, including contingencies, ensures hospitals are prepared for financial surprises, clarifying how much does Epic cost for a hospital.
- Regularly Review Budget Allocations – Monitoring spending against budget allocations helps identify variances early, ensuring better management of how much does Epic cost for a hospital.
Infrastructure Limitations
- Nature of the Challenge – Existing IT infrastructure may not meet Epic’s requirements, leading to operational inefficiencies.
- Potential Solutions:
- Conduct Thorough IT Assessments – Assessing current infrastructure helps determine the upgrades needed, influencing how much does Epic cost for a hospital.
- Invest in Necessary Upgrades – If required, hospitals should invest in cloud solutions to meet scalability needs, factoring into how much does Epic cost for a hospital.
Cybersecurity Concerns
- Nature of the Challenge – New digital systems introduce potential vulnerabilities, increasing cybersecurity risks.
- Potential Solutions:
- Implement Robust Cybersecurity Measures – Establishing strong security protocols before implementation protects sensitive patient data, reducing risks associated with how much does Epic cost for a hospital.
- Conduct Regular Security Audits – Routine audits ensure ongoing system security, further safeguarding how much does Epic cost for a hospital.
User Experience and System Usability
- Nature of the Challenge – Epic’s complex interface can hinder user adoption and efficiency.
- Potential Solutions:
- Gather User Feedback – Involving users during the testing phase helps improve system usability and ensures that how much does Epic cost for a hospital is justified by increased adoption.
- Design Intuitive Workflows – Customizing workflows and dashboards enhances user experience, contributing to maximizing how much does Epic cost for a hospital.
Workplace Culture and Engagement
- Nature of the Challenge – Organizational culture can impact the success of EHR adoption.
- Potential Solutions:
- Encourage a Culture of Learning – Promoting continuous learning helps ease transitions, highlighting the long-term benefits of how much does Epic cost for a hospital.
- Celebrate Small Wins – Recognizing milestones keeps morale high, positively impacting how staff perceive how much does Epic cost for a hospital.
Interdepartmental Collaboration
- Nature of the Challenge – Lack of collaboration between departments can lead to inefficiencies in implementation.
- Potential Solutions:
- Establish Interdisciplinary Teams – Teams from different departments ensure diverse input and improve communication about how much does Epic cost for a hospital.
- Create Open Communication Channels – Open communication between departments enhances transparency, fostering better collaboration in understanding how much does Epic cost for a hospital.
System Optimization Post-Implementation
- Nature of the Challenge: Hospitals may struggle to use Epic to its full potential after implementation.
- Potential Solutions:
- Set Up Ongoing Training – Continued education helps staff leverage Epic’s full capabilities, ensuring how much does Epic cost for a hospital is reflected in effective system use.
- Conduct Regular Performance Evaluations – Reviewing system performance helps optimize usage and identify areas for improvement, directly affecting how much does Epic cost for a hospital.
User Support and Troubleshooting
- Nature of the Challenge – Ongoing technical issues may disrupt workflows and require support.
- Potential Solutions:
- Establish a Dedicated Support Team – A support team can quickly address issues, reducing downtime and justifying how much does Epic cost for a hospital in terms of operational efficiency.
- Implement a Ticketing System – Using a ticketing system to report and resolve issues ensures smooth system operation, contributing to how much does Epic cost for a hospital is managed.
Measuring Impact and Success
- Nature of the Challenge – Difficulty in assessing the EHR system’s effectiveness can hinder improvements.
- Potential Solutions:
- Develop Clear KPIs – Establishing key performance indicators helps measure the system’s impact, providing clear insights into how much does Epic cost for a hospital in terms of success.
- Regularly Review Performance Data – Continuous data review helps refine strategies, ensuring hospitals understand the full implications of how much does Epic cost for a hospital over time.
12. Best Practices for Successful Implementation of Epic
Thorough Planning and Assessment
- Detailed Needs Assessment – Conducting a comprehensive needs assessment before selecting a system ensures that the right features are prioritized. This clarity helps when evaluating how much does Epic cost for a hospital versus other EHR options.
Involving Leadership and Stakeholders
- Executive Sponsorship – Gaining support from hospital leadership is critical for successful implementation. Executives can help communicate the value of understanding how much does Epic cost for a hospital and its benefits across the organization.
Iterative Testing and Feedback Loops
- Phased Rollouts – Implementing Epic in phases allows for user feedback and adjustments, reducing the likelihood of widespread issues. This method helps manage costs associated with how much does Epic cost for a hospital effectively.
Investing in Change Management Strategies
- Change Management Team – Establishing a dedicated team to oversee the change process can provide structured support for staff, enhancing the likelihood of successful adoption.
Post-Implementation Reviews and Continuous Improvement
- Ongoing Feedback Mechanisms – Setting up processes for regular feedback helps ensure that the system continues to meet user needs, maximizing the investment represented by how much does Epic cost for a hospital.
13. Exploring Epic Systems and Other CRM Platforms
Epic Cheers Certification
Epic Cheers Certification is a credential that validates expertise in the Epic Cheers system, a CRM designed specifically for the healthcare industry.
Key Features
- Training Modules – Comprehensive modules cover all functionalities of Epic Cheers, ensuring users are proficient in its use.
- Assessment – A rigorous test that certifies individuals in effectively managing customer relationships through Epic Cheers.
- Professional Recognition – Certification enhances credibility which offers new career opportunities in healthcare organizations.
Importance – Certification in Epic Cheers is vital for professionals managing patient relationships and improving operational efficiency, particularly in healthcare organizations that value specialized CRM capabilities.
Epic Cheers Demo and System
The Epic Cheers Demo provides a real-time demonstration of the system’s features for prospective users and organizations.
Key Features
- Hands-On Experience – Users can explore the interface and functionalities of the Epic Cheers system.
- Use Case Scenarios – Real-world scenarios demonstrate the practical applications of the software in healthcare settings.
- Q&A Session – A live Q&A session helps answer specific questions from participants, providing clarity on system capabilities.
Importance – The demo helps organizations assess whether Epic Cheers fits their CRM needs compared to other platforms like Salesforce. It also highlights the system’s healthcare-focused features, which may be a key differentiator.
Applied Epic CRM
Applied Epic CRM is another CRM platform, originally built for the insurance sector, but gaining traction in healthcare for its robust features.
Key Features
- Comprehensive Data Management: Tools for tracking sales leads, customer interactions, and analyzing metrics.
- Automation Capabilities: Automation to reduce manual work and improve efficiency.
- Integration with Other Systems: Applied Epic CRM integrates accurately with other systems, which can be valuable for multi-industry applications.
Importance – Applied Epic CRM enhances customer relationship management by automating processes, streamlining communications, and improving service delivery, making it a viable option for healthcare organizations alongside Epic Cheers.
Epic Cheers vs. Salesforce
Target Audience
- Epic Cheers: In epic cheers vs salesforce, epic cheers is designed specifically for healthcare providers, focusing on managing patient relationships.
- Salesforce: A general CRM platform with broad industry applications, including healthcare, but not uniquely tailored to it.
Functionality
- Epic Cheers CRM: Offers features and modules customized for healthcare providers, including patient engagement and operational tools.
- Salesforce: A versatile platform that requires customization to meet healthcare-specific needs.
User Experience
- Epic Cheers Module: Known for its intuitive, healthcare-friendly interface that healthcare professionals find easy to navigate.
- Salesforce: A more complex system due to its wide array of features, often requiring extensive training and customization.
14. Virtelligence’s Place in Epic Implementation in Healthcare
Virtelligence is a healthcare IT consulting firm with deep expertise in Electronic Health Record (EHR) systems and service to assist healthcare organizations with implementing Epic and ensuring accuracy and effectiveness.
Strategic Planning and Assessment
- Needs Assessment – Virtelligence conducts comprehensive assessments to understand the specific needs, goals, and current challenges of the healthcare organization.
- Roadmap Development – The firm helps create a detailed strategic roadmap, outlining key milestones, timelines, and resource allocation. This project schedule is essential for efficiently overseeing project stages and managing Epic expenses for a medical facility.
Expert Guidance and Best Practices
- Industry Expertise – Virtelligence’s deep knowledge of Epic systems and healthcare IT allows them to offer best practices and expert advice.
- Customized Solutions – Recognizing the uniqueness of each healthcare provider, Virtelligence tailors its solutions to meet specific needs, improving the effectiveness of Epic in streamlining workflows and enhancing patient care.
Project Management Support
- Dedicated Project Management – Effective Epic implementation requires robust project management. In order to guarantee that the project is completed on schedule and within budget, Virtelligence provides specialized project managers that supervise every step of the implementation process.
- Change Management – Implementing Epic involves significant organizational change. Healthcare firms may reduce worker resistance and guarantee an accurate transition.
Training and Education
- Comprehensive Training Programs – Virtelligence provides extensive training for healthcare staff, ensuring they are well-prepared to use Epic efficiently.
- Ongoing Support – After the initial implementation, Virtelligence continues to provide support, helping staff resolve issues and ensuring they remain proficient with the system, which is essential to sustain the operational improvements.
Data Migration and Integration
- Smooth Data Migration – Migrating data from legacy systems to Epic can be challenging and Virtelligence guarantees an accurate and safe flow of data, protecting data integrity and adherence to healthcare laws.
- System Integration – Virtelligence helps integrate Epic with other critical systems, such as billing, lab information, and scheduling systems. Optimizing hospital workflows and guaranteeing operational efficiency require seamless connection.
Performance Optimization and Evaluation
- Continuous Improvement – After Epic’s implementation, Virtelligence works with healthcare organizations to monitor system performance and identify areas for improvement.
- User Feedback Mechanisms – Virtelligence implements feedback mechanisms to gather insights from end-users. When it comes to post-implementation that enhances system functionality and customer satisfaction then this feedback is priceless.
Regulatory Compliance and Risk Management
- Regulatory Compliance – Ensuring compliance with healthcare standards and regulations, such as HIPAA, is a critical aspect of EHR implementation. Virtelligence ensures that Epic systems meet all necessary regulatory requirements which reduces the risk of compliance issues.
- Risk Management Strategies – Virtelligence helps develop proactive risk management strategies to address potential implementation challenges.
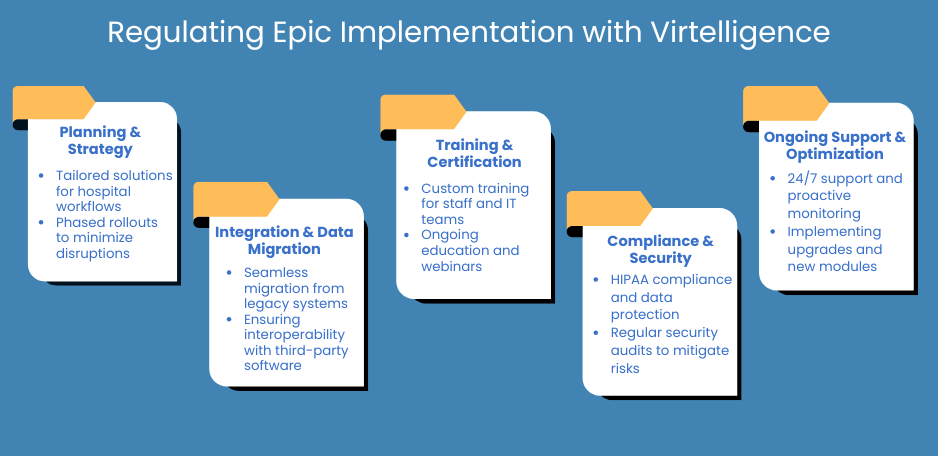
15. Final Thoughts
As hospitals continue to navigate the complex landscape of Electronic Health Record (EHR) systems, understanding how much does Epic cost for a hospital becomes crucial for informed decision-making. The following are some key takeaways for hospital administrators on the real costs of Epic, the future of EHRs, and how to budget for fluctuating expenses:
Summarizing the True Costs of Epic: Key Takeaways for Hospital Leaders
- Initial Investment – The initial costs of implementing Epic can be substantial, including software licensing, hardware, and infrastructure. It’s vital for hospital leaders to be aware of how much does Epic cost for a hospital upfront to budget effectively.
- Ongoing Expenses – Beyond the initial investment, ongoing costs such as maintenance, support, training, and upgrades contribute significantly to the total cost of ownership.
- Total Cost of Ownership (TCO) – Hospital leaders should consider the total cost of ownership when evaluating how much does Epic cost for a hospital. This includes both direct and indirect costs associated with the implementation and long-term operation of the EHR system.
- Return on Investment (ROI) – It is important to weigh the potential return on investment against the costs. Although Epic costs for a hospital might be high initially, the long-term benefits in patient care, efficiency, and compliance can justify the investment.
- Tailored Solutions – Each hospital’s needs are unique. Therefore, understanding how much does Epic cost for a hospital should involve evaluating tailored solutions that align with specific operational requirements and patient care goals.
FAQs
How much does Epic cost for a small hospital?
For small hospitals, the initial cost of implementing Epic’s electronic health record (EHR) system typically ranges between $500,000 to $1 million. This cost covers software licensing, hardware, installation, and setup.
Additionally, hospitals should account for ongoing expenses, including:
- Annual maintenance fees – 15-20% of the original implementation cost.
- Licensing fees – Vary depending on the number of users and specific features.
- Training and support – Costs for educating staff on using the system.
- Upgrades and customizations – As the hospital grows, additional modules may be required.
Are there alternatives to Epic that are more affordable?
Yes, there are several more affordable EHR alternatives to Epic for small hospitals:
- Cerner – A competitor to Epic, offering flexible pricing and a range of solutions.
- Allscripts – Modular options that allow hospitals to select specific functionalities, often making it cost-effective.
- MEDITECH – Well-known for serving smaller hospitals and community clinics with affordable packages.
- Athenahealth – Cloud-based with lower initial costs and scalable pricing for small hospitals.
- NextGen Healthcare – A more affordable EHR system tailored for smaller hospitals and outpatient centers, focusing on essential features like charting, scheduling, and billing.
What are the long-term financial benefits of using Epic?
Although Epic has high initial costs, its long-term financial benefits can be significant:
- Operational Efficiency and Reduced Errors – Epic integrates clinical, administrative, and patient data, streamlining workflows and reducing errors, leading to potential cost savings and reduced liability.
- Improved Revenue Cycle Management – Epic’s integrated billing and revenue cycle management tools enhance billing processes, minimize delays, and improve cash flow.
- Interoperability and Scalability – Epic is highly interoperable, allowing seamless data sharing with other healthcare systems, boosting patient referrals and partnerships.
- Patient Satisfaction and Retention – Epic improves patient engagement through online portals and better communication, leading to higher patient retention and long-term revenue.
- Regulatory Compliance and Incentives – Epic helps hospitals maintain compliance with regulations like HIPAA and qualify for government incentive programs, offering potential financial rewards.