
Healthcare organizations across the United States are increasingly recognizing that Epic EHR success extends far beyond initial implementation. With over 250 healthcare organizations utilizing Epic systems and managing more than 40% of patient records nationwide, the complexity of maintaining optimal performance has grown exponentially.
Your Epic investment represents more than technology; it’s the backbone of patient care delivery, operational efficiency, and financial performance. However, the question isn’t whether your organization can manage Epic internally, but whether you should be dedicating precious resources to this complex undertaking when specialized partners can deliver superior results.
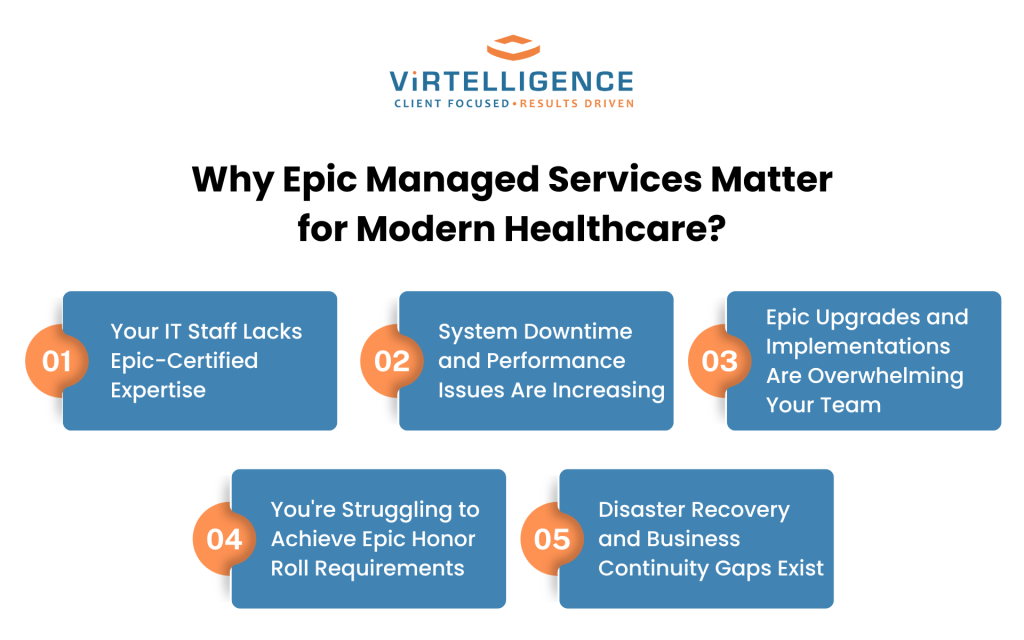
Why Epic Managed Services Matter for Modern Healthcare?
Epic systems have transformed healthcare delivery, but they’ve also introduced unprecedented complexity into hospital operations. The platform’s comprehensive nature—spanning clinical workflows, revenue cycle management, population health, and patient engagement—requires specialized expertise that extends well beyond traditional IT support.
Modern healthcare organizations face a critical decision point. You can continue stretching internal resources to manage increasingly complex Epic environments, or you can partner with specialized managed services providers who live and breathe Epic optimization daily. The difference between these approaches often determines whether your Epic investment becomes a competitive advantage or an operational burden.
Consider this: while your clinical teams focus on patient care and your administrators manage healthcare delivery, Epic managed services partners dedicate their entire organizational capacity to maximizing EHR performance, ensuring compliance, and staying ahead of system updates and industry requirements.
Sign #1: Your IT Staff Lacks Epic-Certified Expertise
The most telling indicator that your hospital needs an Epic managed services partner is when your IT team struggles with Epic-specific challenges that require certified expertise to resolve effectively.
Epic certification isn’t just a credential—it’s a comprehensive knowledge framework that takes months to achieve and requires ongoing maintenance to remain current. Each Epic module demands specialized understanding, from Hyperspace and MyChart to revenue cycle components like Professional Billing and Hospital Billing.
The Cost of Epic Certification Training
Epic certification programs can cost between $3,000 $8,000 per person, depending on the module and training track. More significantly, the time investment is substantial—most certification programs require 2-4 weeks of intensive training followed by hands-on experience under certified supervision.
For a mid-sized hospital system, maintaining a full complement of Epic-certified staff across all necessary modules can easily exceed $200,000 annually in training costs alone. This doesn’t account for the productivity loss during training periods or the ongoing education required to maintain certifications.
Staffing Turnover Challenges in Healthcare IT
Healthcare IT professionals with Epic expertise command premium salaries, often 20-30% above standard IT roles. This creates two challenges: higher ongoing costs and increased turnover risk as certified professionals become highly sought after by competing organizations.
When Epic-certified staff leave, you’re not just losing an employee—you’re losing institutional knowledge about your specific Epic configuration, customizations, and workflows. Replacing this expertise can take 6-12 months and costs significantly more than maintaining continuous expert support through managed services partnerships.
Sign #2: System Downtime and Performance Issues Are Increasing
Epic system reliability directly impacts patient care quality and organizational efficiency. If you’re experiencing more frequent downtimes, slower system response times, or user complaints about system performance, these issues indicate that your current support model isn’t meeting Epic’s operational demands.
Healthcare organizations report that every hour of Epic downtime can cost between $50,000 to $100,000 in lost productivity, delayed procedures, and administrative inefficiencies. More critically, system unavailability during patient care can compromise safety and outcomes.
Impact of System Downtime on Patient Care
When Epic systems experience outages or performance degradation, clinical workflows immediately suffer. Physicians can’t access patient records, nurses can’t document care delivery, and pharmacists can’t verify medication orders. These disruptions don’t just affect efficiency; they can compromise patient safety.
Epic managed services partners maintain dedicated infrastructure monitoring and rapid response capabilities that most hospitals can’t justify internally. They utilize advanced monitoring tools, predictive analytics, and proactive maintenance schedules to prevent issues before they impact operations.
24/7 Monitoring Requirements
Epic systems require continuous oversight, but most hospitals can’t afford round-the-clock internal IT staffing. Epic managed services providers offer true 24/7/365 monitoring with escalation protocols designed specifically for healthcare environments.
This continuous monitoring includes database performance optimization, interface monitoring, system resource utilization, and proactive identification of potential issues. When problems arise, certified experts can often resolve them remotely before they impact end users or patient care delivery.
Sign #3: Epic Upgrades and Implementations Are Overwhelming Your Team
Epic releases major upgrades twice yearly, and each upgrade introduces new features, security enhancements, and potential compatibility challenges. If your team dreads Epic upgrade announcements or struggles to complete implementations within reasonable timeframes, you need specialized support.
Epic upgrades aren’t optional; they’re essential for maintaining security, compliance, and access to new features that improve patient care and operational efficiency. However, managing these upgrades while maintaining day-to-day operations requires expertise and resources that many organizations lack internally.
Resource Planning for Epic Version Upgrades
Successful Epic upgrades require comprehensive planning, testing, and validation processes that can consume 3-6 months of dedicated effort from certified resources. This includes impact analysis, customization review, interface testing, user training, and go-live support.
Epic managed services partners maintain dedicated upgrade teams who manage multiple client upgrades throughout the year. They understand common pitfalls, have established testing methodologies, and can complete upgrades more efficiently than internal teams learning these processes on an annual basis.
Hardware and Infrastructure Compatibility Issues
Each Epic upgrade may introduce new hardware requirements, database optimization needs, or infrastructure compatibility challenges. Epic managed services partners maintain current knowledge of hardware requirements and can ensure your infrastructure remains optimized for Epic performance.
They also maintain relationships with hardware vendors and can leverage bulk purchasing power to help you achieve cost-effective infrastructure upgrades when necessary.
Sign #4: You’re Struggling to Achieve Epic Honor Roll Requirements
Epic’s Honor Roll recognition represents the highest level of Epic utilization and optimization. If your organization isn’t achieving Honor Roll status or maintaining these standards consistently, you’re likely missing opportunities to maximize your Epic investment’s value.
Honor Roll achievement requires maintaining specific performance metrics across clinical adoption, patient engagement, care quality, and technical optimization. These metrics go beyond basic system functionality to measure how effectively your organization leverages Epic’s full capabilities.
Understanding Epic Honor Roll Criteria
Honor Roll recognition requires meeting or exceeding benchmarks in areas including MyChart activation rates, provider efficiency metrics, clinical decision support utilization, and population health management capabilities. These metrics require specialized analysis and optimization strategies that extend beyond traditional IT support.
Epic managed services partners understand these requirements intimately and can help you develop strategies to achieve and maintain Honor Roll status. They bring experience from multiple client implementations and can share best practices for optimizing performance across all measured areas.
Performance Metrics and Reporting Requirements
Achieving Honor Roll status requires sophisticated reporting and analytics capabilities to track performance metrics continuously. This includes custom report development, dashboard creation, and ongoing analysis of system utilization patterns.
Epic managed services providers maintain dedicated analytics teams who understand Epic’s reporting capabilities and can develop the monitoring and reporting infrastructure necessary to track Honor Roll metrics effectively.
Sign #5: Disaster Recovery and Business Continuity Gaps Exist
Healthcare organizations can’t afford Epic system failures during critical operations. If your disaster recovery planning for Epic systems feels inadequate or untested, you’re exposing your organization to significant operational and financial risks.
Epic disaster recovery isn’t just about data backup—it requires comprehensive business continuity planning that includes failover procedures, data synchronization, user access management, and rapid recovery protocols specifically designed for healthcare environments.
HIPAA Compliance in Disaster Recovery
Epic disaster recovery solutions must maintain HIPAA compliance throughout all backup, recovery, and failover processes. This requires specialized expertise in healthcare data protection regulations and Epic-specific security configurations.
Epic managed services partners maintain HIPAA-compliant disaster recovery solutions that include encrypted data transmission, secure backup storage, and documented recovery procedures that meet regulatory requirements. They also conduct regular recovery testing to ensure systems can be restored within required timeframes.
Recovery Time Objectives (RTOs) for Critical Systems
Healthcare organizations typically require Epic system recovery within 2-4 hours of any major outage. Achieving these aggressive RTOs requires sophisticated disaster recovery infrastructure and procedures that most hospitals can’t maintain cost-effectively internally.
Epic managed services providers can offer guaranteed RTOs backed by redundant infrastructure, automated failover capabilities, and dedicated recovery teams available around the clock.
The Strategic Value of Partnering with Epic Managed Services Experts
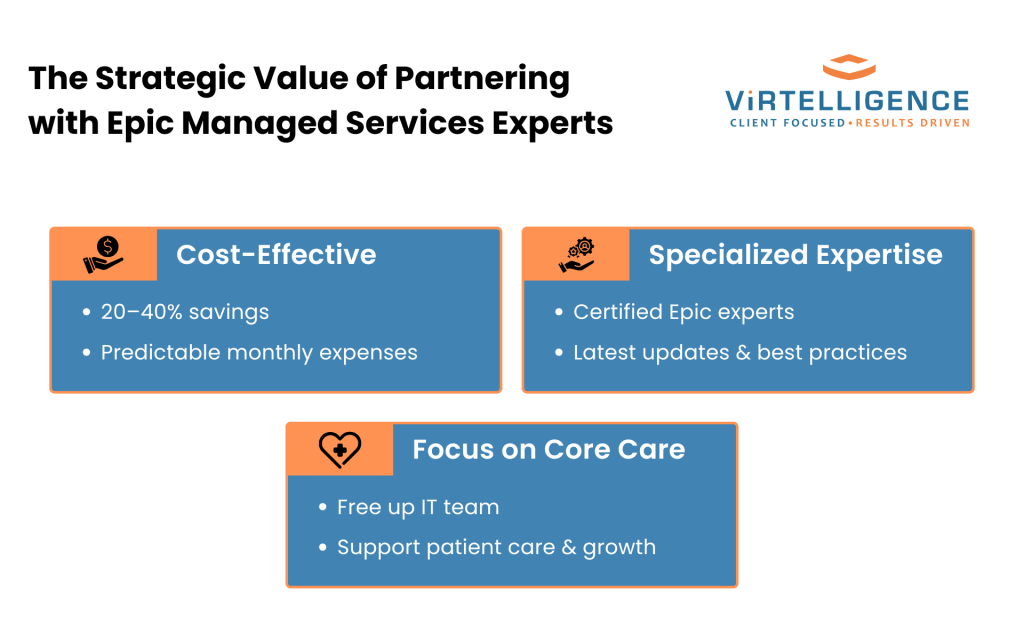
Rather than viewing Epic managed services as an additional expense, forward-thinking healthcare leaders recognize these partnerships as strategic investments that deliver measurable returns across multiple dimensions.
Epic managed services partnerships allow your internal IT team to focus on strategic initiatives that directly support your organization’s mission rather than spending time on routine maintenance and support activities that specialized providers can handle more efficiently.
Cost-Effectiveness of Managed Services
While managed services partnerships require ongoing investment, they typically deliver 20-40% cost savings compared to maintaining equivalent internal capabilities. These savings come from eliminated recruitment costs, reduced training expenses, shared infrastructure investments, and improved operational efficiency.
More importantly, managed services partnerships convert variable costs into predictable monthly expenses, making IT budgeting more straightforward and eliminating the financial surprises that can accompany major system issues or upgrade requirements.
Access to Specialized Epic Expertise
Epic managed services providers maintain teams of certified experts across all Epic modules and specializations. This gives your organization immediate access to expertise that would take years and significant investment to develop internally.
These experts stay current with Epic developments, participate in user group meetings, and maintain relationships with Epic that provide early insight into upcoming changes and best practices. This expertise benefits your organization without requiring direct investment in ongoing education and certification maintenance.
Focus on Core Healthcare Operations
Perhaps most importantly, Epic managed services partnerships allow your leadership team and internal IT resources to focus on initiatives that directly support patient care delivery and organizational growth rather than spending time on system maintenance and technical support activities.
This strategic focus enables better alignment between technology investments and organizational objectives, leading to improved outcomes across clinical, operational, and financial metrics.
How to Choose the Right Epic Managed Services Partner?
Selecting an Epic managed services partner requires careful evaluation of expertise, experience, and cultural fit with your organization’s values and objectives.
Look for partners who maintain extensive Epic certifications, demonstrate experience with organizations similar to yours, and can provide references from current clients who can speak to their performance and reliability.
Key Qualifications to Look For
Essential qualifications include current Epic certifications across relevant modules, demonstrated experience with Epic upgrades and implementations, proven disaster recovery capabilities, and strong references from healthcare clients.
Additionally, evaluate their monitoring and reporting capabilities, escalation procedures, and ability to provide detailed performance metrics that align with your organization’s objectives and requirements.
Questions to Ask Potential Partners
Critical questions include: How do you maintain Epic certifications across your team? What are your guaranteed response times for different types of issues? How do you handle Epic upgrades, and what is your track record for on-time, on-budget completion? Can you provide detailed references from similar healthcare organizations?
Also, ask about their disaster recovery testing procedures, security protocols, and how they stay current with Epic developments and best practices.