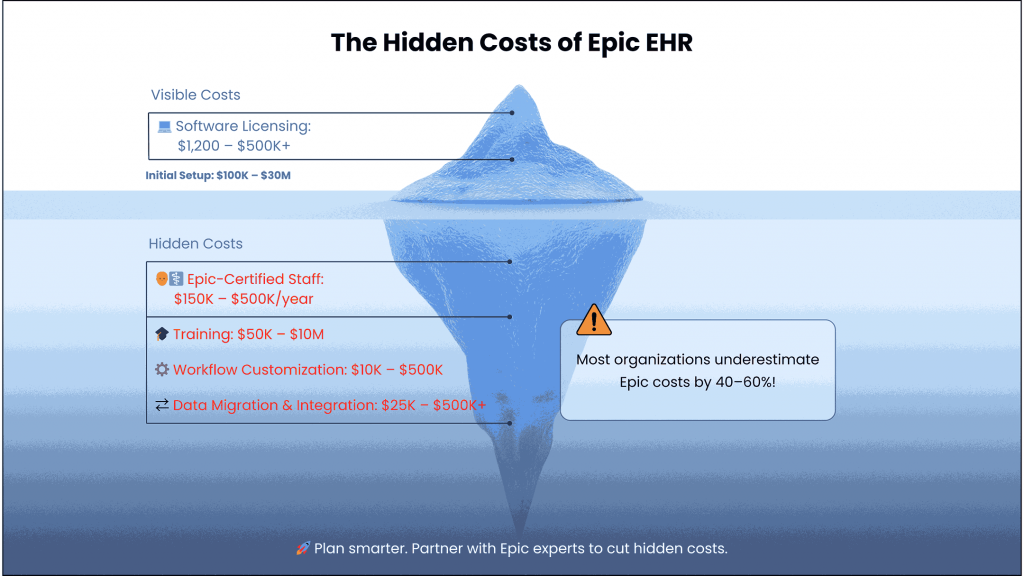
When healthcare leaders evaluate Epic EHR implementation, the conversation often begins with the visible price tag, software licensing fees ranging from $1,200 for small practices to over $500,000 for large hospital systems. However, these upfront costs represent only the tip of the financial iceberg.
The reality? Organizations typically underestimate their total Epic investment by 40-60%, with hidden expenses emerging throughout implementation and ongoing operations. These overlooked costs can transform what appears to be a manageable IT investment into a multi-million dollar commitment that strains budgets and resources for years.
Understanding Epic’s complete financial picture isn’t just about better budgeting; it’s about making strategic decisions that align with your organization’s long-term operational and financial health.
The Complete Epic Implementation Cost Breakdown
Initial Investment Components
Epic’s implementation costs vary dramatically based on organizational size and complexity. Small practices might invest $100,000-$300,000 in setup costs, while large hospital systems face initial investments ranging from $10 to $30 million. These figures encompass several critical components that extend far beyond software licensing.
Software Licensing Structure: Epic’s licensing model creates the foundation for all other costs. Physician licenses typically cost $5,000-$7,000 annually, while clinical staff licenses range from $3,000-$5,000. Even read-only access carries costs of $500-$1,000 per user. For a mid-sized practice with 15 physicians and 25 support staff, annual licensing alone can exceed $150,000.
Infrastructure and Hardware Requirements: Epic demands a robust technical infrastructure to function effectively. Organizations must often upgrade their core network architecture, wireless infrastructure for mobile access, and internet bandwidth to ensure optimal performance. These infrastructure improvements typically represent 15-25% of the total implementation budget, with costs ranging from $50,000 for small practices to several million for large health systems.
Data Migration and System Integration: Converting years of patient records and integrating with existing systems requires specialized expertise. Data migration costs vary significantly based on the volume of historical records and complexity of existing systems, typically ranging from $25,000 for small practices to over $500,000 for large hospital networks.
Hidden Implementation Expenses Most Organizations Miss
The most significant budget surprises emerge from expenses that aren’t immediately obvious during initial Epic evaluations. These hidden costs often represent the difference between a successful implementation and a financial disaster.
Epic-Certified IT Staffing Requirements: Epic cannot be supported with generic IT personnel. Organizations must build teams of Epic-certified analysts, application coordinators, and report writers—premium-salaried positions in a highly competitive market. Annual staffing costs for dedicated Epic support teams range from $150,000-$500,000, depending on organization size and scope of responsibilities.
The challenge extends beyond salary costs. Epic-certified professionals command 20-40% higher salaries than their non-certified counterparts, and retention becomes critical as these individuals become intimately familiar with your organization’s specific Epic configuration.
Comprehensive Training Programs: Effective staff training represents one of the most underestimated expenses. Large health systems should budget $2-10 million for initial training programs, while smaller organizations typically invest $50,000-$200,000. These costs cover initial go-live training, ongoing education programs, and developing internal “super-users” who can provide peer support.
Training extends beyond clinical staff to include administrative personnel, executives, and even board members who need to understand Epic’s capabilities and limitations for strategic decision-making.
Workflow Customization and Configuration Costs: While Epic offers extensive out-of-the-box functionality, most organizations require significant customization to match their specific workflows. Customization costs can range from $10,000 for minor modifications to several hundred thousand dollars for complex, organization-specific requirements.
The key insight? Organizations that prioritize standardization before customization typically reduce these costs by 25-30% while achieving faster implementation timelines.
The Ongoing Operating Expense Reality
Epic’s implementation marks the beginning, not the end, of your financial commitment. Ongoing operational expenses often exceed initial projections, creating long-term budget pressures that many organizations fail to anticipate.
Annual Maintenance and Support Fees
Standard Maintenance Costs: Epic charges approximately 20% of initial licensing costs annually for maintenance and support services. For an organization with $500,000 in initial licensing, annual maintenance fees reach $100,000. These fees cover software updates, technical support, and access to Epic’s knowledge base and training resources.
Software Updates and Version Upgrades: Epic periodically releases major system updates that require significant organizational investment. Upgrade costs typically range from $100,000 to $500,000, depending on implementation complexity and organizational size. These upgrades often necessitate additional staff training and workflow adjustments, creating cascading expenses throughout the organization.
Technical Support and Help Desk Services: Beyond Epic’s standard support, many organizations require dedicated help desk services to support daily operations. Internal help desk staffing costs range from $75,000-$150,000 annually, while outsourced support services typically cost $50,000-$100,000 per year.
Staffing and Human Resources Costs
Epic-Certified Analyst Salaries and Retention: Epic-certified analysts command premium salaries that continue rising as demand outpaces supply. Application analysts typically earn $80,000-$120,000 annually, while senior Epic consultants can command $150,000-$200,000 or more. Retention becomes critical as turnover can cost 50-200% of annual salary in recruiting and retraining expenses.
Ongoing Training and Certification Maintenance: Epic certifications require regular renewal and continuing education. Organizations should budget $5,000-$10,000 per certified employee annually for training, certification maintenance, and professional development. This investment is essential for maintaining Epic support capabilities and staying current with system updates.
Productivity Loss During Transition: Healthcare organizations experience well-documented productivity declines of 15-25% during the first 3-6 months post-implementation. For a practice generating $10 million annually, this productivity loss represents $375,000-$625,000 in potential revenue impact during the transition period.
Infrastructure and Technology Refresh Cycles
Hardware Replacement Requirements: Epic environments require regular hardware refreshes on 3-5 year cycles. Server, storage, and end-user device replacements represent recurring capital expenses that must be modeled as ongoing costs. Organizations should budget 5-10% of initial hardware investment annually for replacement and upgrade cycles.
Network and Security Infrastructure Upgrades: Healthcare cybersecurity requirements continue evolving, necessitating regular network and security infrastructure improvements. Annual security and network upgrade costs typically range from $25,000-$100,000, depending on organizational size and complexity.
Cloud Storage and Data Management Costs: Epic implementations generate massive amounts of data requiring secure storage and management. Cloud storage costs grow continuously, with organizations typically spending $10,000-$50,000 annually on data storage and backup services.
Total Cost of Ownership: The 10-Year Financial Impact
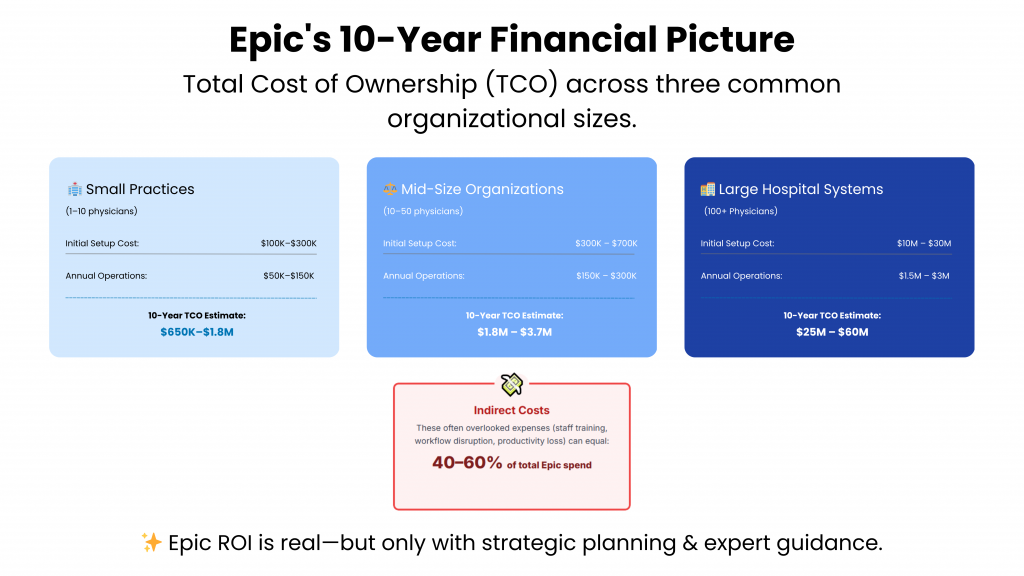
Understanding Epic’s true financial impact requires examining Total Cost of Ownership (TCO) over extended periods, typically calculated over 10-year timeframes for strategic planning purposes.
Epic TCO by Organization Size
Small Practices (1-10 Physicians)
- Initial Setup: $100,000-$300,000
- Annual Operating Costs: $50,000-$150,000
- 10-Year TCO: $650,000-$1,800,000
Mid-Size Organizations (10-50 Physicians)
- Initial Setup: $300,000-$700,000
- Annual Operating Costs: $150,000-$300,000
- 10-Year TCO: $1,800,000-$3,700,000
Large Hospital Systems (100+ Physicians)
- Initial Setup: $10-30 Million
- Annual Operating Costs: $1.5-3 Million
- 10-Year TCO: $25-60 Million
Direct vs. Indirect Cost Analysis
Direct costs include obvious expenses like licensing, hardware, and implementation services. However, indirect costs often represent 40-60% of total Epic investment and include opportunity costs, productivity impacts, and organizational change management expenses.
Indirect costs prove particularly challenging to quantify but significantly impact organizational financial health. These include executive time spent on Epic-related decisions, staff overtime during implementation periods, and potential revenue loss from implementation-related disruptions.
The Hidden Productivity and Workflow Costs
Epic’s complexity creates ongoing productivity challenges that generate hidden costs throughout its operational lifecycle.
Staff Training and Adaptation Challenges
Learning Curve Impact on Patient Care Epic’s extensive functionality requires significant learning time for clinical staff. During the adaptation period, appointment times may increase, documentation takes longer, and staff satisfaction often declines. These factors can impact patient satisfaction scores and, potentially, reimbursement rates tied to quality metrics.
Super-User Development and Support Requirements Successful Epic implementations rely heavily on internal “super-users” who provide peer support and training. Developing and maintaining super-user programs requires ongoing investment in staff time and training resources, typically representing 2-5% of total annual Epic costs.
Ongoing Education and Skill Development Epic’s regular updates and new feature releases require continuous staff education. Organizations should budget for ongoing training programs, user conferences, and certification maintenance to maximize their Epic investment value.
System Customization and Integration Expenses
Third-Party Application Connections: Most healthcare organizations require Epic integration with specialized software for radiology, laboratory services, or practice management. Integration costs vary widely but typically range from $15,000-$75,000 per connection, with ongoing maintenance costs of $5,000-$15,000 annually.
Legacy System Migration Costs: Organizations with extensive legacy systems face complex migration challenges. Complete system migrations can cost $100,000-$500,000, while maintaining parallel systems during transition periods adds significant operational complexity and cost.
API Development and Maintenance: Custom API development for unique organizational requirements typically costs $25,000-$100,000 initially, with ongoing maintenance representing 15-20% of development costs annually.
Comparing In-House vs. Outsourced Epic Management
The decision between internal Epic management and outsourced solutions significantly impacts long-term costs and operational effectiveness.
The True Cost of Internal Epic Teams
Building internal Epic capabilities requires substantial investment in recruitment, training, and retention. Full-time Epic-certified staff provide deep organizational knowledge but represent significant ongoing commitments. Internal teams also face challenges staying current with Epic updates and best practices without substantial continuing education investments.
Alternative Staffing Models and Their ROI
Strategic partnerships with specialized Epic consulting firms can provide access to deep expertise without the full cost of internal teams. Flexible staffing models allow organizations to scale Epic support based on current needs while maintaining access to specialized knowledge for complex projects or system upgrades.
Hybrid approaches combining core internal staff with consulting support for specialized projects often provide optimal cost-effectiveness while ensuring continuity of Epic operations.
Strategic Cost Optimization Approaches
Healthcare organizations can significantly reduce Epic’s total cost of ownership through strategic planning and implementation approaches.
Proven Methods to Reduce Epic TCO
Standardization Before Customization Strategy: Organizations that prioritize Epic’s standard workflows before implementing customizations typically achieve 25-30% cost reductions and faster implementation timelines. This approach allows staff to learn Epic’s intended workflows before modifications, reducing training complexity and ongoing support requirements.
Phased Implementation Planning: Implementing Epic modules in phases spreads costs over extended periods and allows organizations to realize benefits from initial modules while planning subsequent implementations. Phased approaches also reduce organizational change management challenges and associated productivity losses.
Strategic Partnership Leveraging: Collaborating with experienced Epic consulting partners can accelerate implementations, reduce common mistakes, and provide access to best practices developed across multiple organizations. These partnerships often pay for themselves through avoided implementation delays and reduced rework costs.
Long-Term Financial Planning Best Practices
Successful Epic implementations require comprehensive financial planning that extends far beyond initial implementation. Organizations should develop 10-year budget models that account for upgrade cycles, staff growth, and evolving technology requirements.
Regular TCO reviews help organizations identify cost optimization opportunities and ensure Epic continues delivering expected value. These reviews should examine both direct costs and indirect impacts on organizational productivity and patient satisfaction.
Making the Business Case: ROI vs. Total Investment
Despite substantial costs, Epic can deliver a significant return on investment when properly implemented and managed.
Quantifying Epic’s Value Proposition
Epic implementations typically deliver measurable improvements in clinical quality, operational efficiency, and regulatory compliance. Organizations often realize 10-15% improvements in billing accuracy, 20-30% reductions in chart retrieval time, and significant improvements in quality reporting capabilities.
These benefits, when quantified over Epic’s operational lifetime, often justify the substantial investment required. However, realizing these benefits requires strategic implementation planning and ongoing optimization efforts.
When Epic Makes Financial Sense
Epic’s comprehensive capabilities make financial sense for organizations with sufficient scale and complexity to utilize its extensive functionality. Organizations with fewer than 10 physicians often struggle to justify Epic’s costs, while those with 25+ physicians and multiple locations typically find Epic’s capabilities align well with their operational requirements.
The decision should consider not just current needs but anticipated growth and evolving healthcare requirements. Epic’s scalability can support organizational growth without requiring EHR system changes, providing long-term strategic value.
Conclusion: Planning for Epic’s True Financial Impact
Epic EHR implementation represents one of healthcare’s most significant technology investments, with total costs often exceeding initial projections by 40-60%. Understanding these hidden costs enables better financial planning and more realistic ROI expectations.
The key to Epic’s success lies not in minimizing costs but in strategic planning that accounts for Epic’s complete financial impact while maximizing its substantial capabilities. Organizations that approach Epic implementation with comprehensive financial models, realistic timelines, and strategic partnerships typically achieve better outcomes and stronger returns on their investments.
Consider partnering with healthcare IT experts who understand Epic’s complexities and can help your organization navigate implementation challenges while optimizing your technology investment. Strategic consulting partnerships often pay for themselves through improved implementation efficiency and reduced long-term operational costs.
Ready to explore how strategic Epic planning can optimize your healthcare IT investment? Let’s discuss your organization’s specific needs and develop a comprehensive approach that maximizes value while managing costs effectively.