Introduction
Overview of EHR Migration
Definition and Importance of EHR (Electronic Health Records)
Electronic Health Records (EHRs) have reshaped healthcare, making EHR migration an essential part of this transformation. EHRs have turned patients’ paper charts into digital files.
These files can store vast amounts of information, like:
- Complete medical histories
- Accurate diagnoses
- Medication lists
- Customized treatments
- Current vaccination records
- Known allergies
- Clear radiology images
- Precise lab results
This digital shift ensures straightforward sharing of data across many healthcare settings and offers immediate, secure access to patient-focused records for authorized users only.
The benefits of Electronic Health Records (EHRs) extend far beyond simply going digital. By providing quick and efficient access to patient records, EHRs help sharpen medical diagnoses. They also reduce medical mistakes and make it easier to manage long-term health issues.
Also, EHRs are key to the safe exchange of information among healthcare providers. This leads to better-organized care processes and in the end, improved patient results.
Reasons for Migrating EHR Systems
Technology is getting better. Healthcare organizations sometimes have to change from old EHR systems to ones that are better, quicker and have more features. There are a few reasons why changes to EHR systems happen.
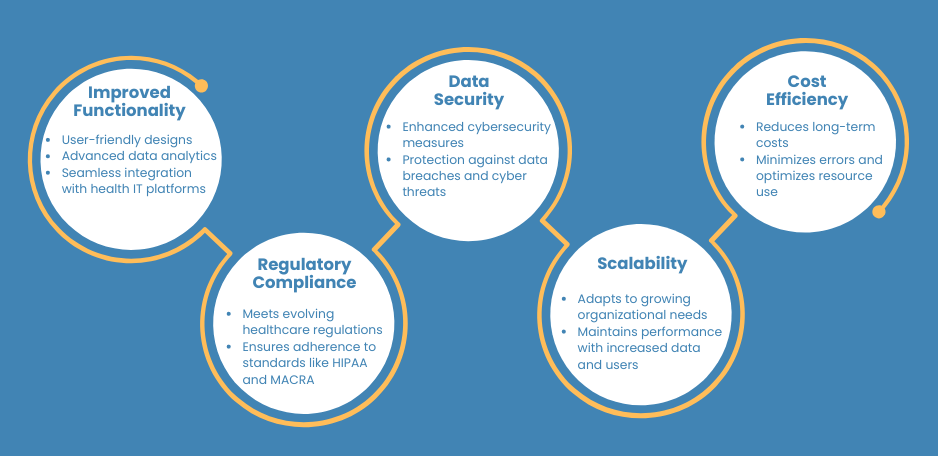
- Improved Functionality: In the realm of modern Electronic Health Record (EHR) systems, the advancements are truly remarkable. The examples include:
- User-Friendly Interfaces: Making navigation faster and simpler with clear interfaces.
- Smart Data Analytics: Utilizing tools to foresee results and spot health risks.
- Compatibility: Effortless exchanging data across numerous medical IT platforms.
- Regulatory Compliance: Healthcare regulations are constantly evolving, with stringent standards like HIPAA and MACRA dictating the industry’s compliance requirements. To deal with this situation well, healthcare providers need to keep their EHR systems current. Their systems must follow these guidelines. This helps them follow the rules, keep data safe, and provide top-level healthcare.
- Data Security: We live in a digital world. So we must protect our patients’ information through EHR migration to modern systems. That’s why modern EHR systems come with top-notch, strong protection. They help fight against dangers on the internet and data leaks. Using strict safety steps helps keep sensitive health data secret, intact and available. This builds trust between patients and providers.
- Scalability: EHR migration ensures that EHR systems can change in size for growing healthcare organizations. If your organization is getting bigger, the system must grow smoothly to manage more data and users. And, it can’t harm how it works. A flexible EHR system helps organizations keep up with changes while keeping work smooth and data safe.
- Cost Efficiency: If you move to a better EHR system, EHR migration can save a lot of money in the future. You can cut down office costs, lessen mistakes, and better use resources. This smoothes work and improves finances. Using a cost-friendly EHR solution not only improves work but also improves how care is given.
Objectives of the Guide
What Readers Will Learn
This guide is your map to a successful EHR migration journey. You’ll learn:
- How important it is to plan and assess before you start the EHR migration.
- How to find the EHR system that matches your organization’s aim.
- The right way to prepare and move data safely and correctly.
- Training your team for the best use and understanding of the EHR system.
- Checking and confirming the new EHR system for reliability and rules.
- Starting with a good EHR migration plan to avoid issues and face any problems.
- Getting continual support for a better performing EHR system.
Importance of Following Best Practices
Ensuring a smooth EHR migration is important for several reasons:
- Minimizing Disruptions: A carefully thought out EHR migration means no interruptions in healthcare services. This ensures patients aren’t affected during the shift.
- Ensuring Data Integrity: A step-by-step data plan and strict transfer protocols prevent data loss, corruption, or inaccuracies. This maintains the integrity of essential health information.
- Enhancing User Adoption: Teaching users thoroughly and managing change helps people accept and become skilled with the new EHR system. This leads to better system use.
- Mitigating Risks: Testing, validating, and checking security in good ways allows for early spotting and solving problems during EHR migration, which lowers the chance of system breakdowns and going against rules.
- Achieving Long-Term Success: Regular monitoring, support, and adjustment means that the EHR system changes with the organization’s needs. This offers lasting value and better healthcare results.
Getting to know EHR migration is essential. Understanding the importance of moving Electronic Health Records (EHRs) and having a good grasp of what this guide aims to achieve empowers readers to start refining their EHR systems.This improvement mission seeks to raise not only how well and how efficiently patients are cared for, but also to make processes neater, data easier to access, and advanced tech smooth to incorporate within healthcare spaces.
1. Planning Your EHR Migration
Initial Assessment and Feasibility
Evaluating Current Systems and Needs
Think of preparing your EHR migration plan like examining a road map. Start by deeply understanding your current position.
- Assess Your Current EHR Setup: Identify what’s working and what’s not. Recognize the specific needs of your organization.
- Conduct a Detailed Study: This helps decide if moving to a new EHR system makes sense and defines what’s needed for success.
A careful evaluation is the foundation for a smooth EHR migration, ensuring the new system meets your organization’s unique challenges and goals.
Budgeting and Financial Planning
Financial Planning for EHR Migration
Switching to a new EHR system needs good financial management. For a smooth, cost-efficient EHR migration, follow these steps:
- Calculate Overall Costs:
- Software: Determine the price for new EHR software.
- Hardware: Budget for necessary hardware upgrades.
- Data Transition: Estimate costs for transferring existing data.
- Training: Allocate funds for employee training on the new system.
- Maintenance: Plan for ongoing maintenance expenses.
- Create a Detailed Budget:
- Track all expenses meticulously to avoid surprises.
- Ensure every financial aspect is accounted for to prevent project delays.
- Secure Adequate Funding:
- Obtain sufficient funding to cover all anticipated costs.
- Use resources wisely to maximize value and minimize waste.
- Plan for Contingencies:
- Set aside a contingency fund to handle unexpected expenses.
- Routinely check and adjust your budget to stay on course.
By following these careful steps, you can ensure a smooth and cost-effective EHR migration.
Setting Clear Objectives
Defining Goals and Success Metrics
EHR migration can be tricky. Yet, starting with clear, well-defined goals makes everything easier and more productive. Here’s how to set clear objectives:
- Align with Strategy: Ensure goals support your organization’s mission. This helps secure support and resources.
- Measure Success: Monitor success with dedicated measurements to boost patient care, data safety, and operations.
- Create a Roadmap: Clear goals and metrics guide your migration, increasing the chances of success.
Setting clear goals and monitoring progress guarantees a seamless, effective EHR migration, which benefits your organization and patients.
Aligning Objectives with Organizational Strategy
For a successful EHR migration, make certain your process goes hand-in-hand with your organization’s big-picture goals. This ensures that the fresh EHR system fits current needs and promotes long-term progress. Let’s say your main goal is to increase patient involvement. Your EHR migration plan should then highlight features that allow easy interaction with patients and health record access. By tying together objectives of EHR migration with your organization’s bigger vision, the migration boosts advantages that last and improves operations and results.
Stakeholder Involvement
Identifying Key Stakeholders
EHR migration can be a complicated task. It needs lots of people from different areas in your company to play an active part. Some of these people are:
- Healthcare professionals who give patient care.
- Office staff who coordinate work processes.
- IT specialists who take care of system integration.
- Leaders who make critical choices.
If you find and include these people early in the change, teamwork shines.
This team setting lets them think about different views, needs, and wants. These people, because of their different jobs and know-how, give helpful thoughts.
They spot problems ahead and make sure that the EHR migration works well with the real-life and vital goals of the organization. Having their help and ideas is key to making the change happen and the new EHR system works well.
Engaging Leadership and Staff
Your EHR migration success leans heavily on backing from both leadership and staff. Getting leaders onboard does more than show authority, it also earmarks crucial resources needed to drive the EHR migration project forward.
Plus, including staff members, particularly those who will be using the new system, promotes ownership, encourages involvement, and eases resistance to change. Smooth EHR migration hinges on strong communication strategies. Keeping everyone in the loop with regular updates and feedback sessions is key during the EHR migration voyage.
This team-focused and open method sparks a culture of dedication and responsibility among team members, smoothing the path for change and raising the success rate.
By carefully mapping out your EHR migration, doing in-depth feasibility checks, setting clear goals, and engaging important stakeholders, you’re dropping sturdy building blocks for EHR migration that fits your organizations needs and boosts overall work efficiency.
2. Choosing the Right EHR System
Evaluating Options
Criteria for Selection
Picking a fitting EHR system for your health organization is major in EHR migration. Careful, specific selection is needed. Criteria to check includes:
- Functionality: Look at each EHR system’s features and abilities. A top-notch EHR system boosts normal workflows, patient handling, billing, and other important tasks without causing interference. It makes processes quick, enhancing patient service and overall effectiveness.
- Usability: For health care providers, easy-to-use interfaces and intuitive design are vital. They help them adopt and fully use EHR systems faster. A difficult EHR interface can delay work, bother team members, and lower the standard of patient service. Aim for EHR systems that are simple to use and need less training.
- Interoperability: Merging with various health IT systems, like lab information systems, pharmacy systems, and imaging systems, is key for smooth EHR migration. Interoperable EHR systems allow fast and correct data sharing across platforms, ensuring ongoing care and full access to patient details.
- Vendor Support: While picking an EHR system, strong vendor support and training are important. Constant help from the vendor can solve problems quickly, making sure the system works at its best for your organization. Think about the presence and quality of vendor support during and after the start-up phase.
- Cost: It’s key to examine the whole cost of ownership when investing in an EHR system. Besides the initial setup costs, look at costs for training, upkeep, and any extra fees. Knowing these aspects will help you understand the system’s real worth and how it affects your organization’s financial future.
Vendor Comparison and Selection Process
Start your EHR migration by determining what you need. Now, how do you choose the right vendor? Here’s what you do:
- Researching Vendors: The first step is to gather information about vendors. Find the EHR vendors that might suit you. Read online reviews, look up reports in the healthcare field, and ask others in the healthcare world for their suggestions. Your goal should be to make a list of good vendors known for their solid work.
- Requesting Proposals: Once you have narrowed down your list, contact those vendors. Ask for their complete proposals. What should be in the proposals? Information about the system’s features, how you can customize it, when you can have it, and training programs for your staff. Also, details about the support they offer and the total cost, with no hidden surprises.
- Demonstrations: Arrange for demonstrations. These could be live or virtual. This way, you can see how the EHR system works. You can check out the user-friendly interface, the functionality, and the ease of entering data. Plus, you get a sense of how well it fits with your organization’s work style and specific needs. Look for those special features that might just be what your practice needs and make sure it all syncs with your current systems.
- Reference Checks: Before deciding, conduct thorough reference checks. Contact other healthcare groups. Ask them about the EHR systems you’re considering. Get feedback on system performance and how responsive and reliable the vendors were. Consider how easy it was to integrate the system. Check out data safety measures. Ask about challenges during the EHR migration process. This step provides valuable insights and pitfalls to avoid in the EHR migration journey.
- Decision-Making: Based on evaluations, pick the EHR system that best fits with your organization’s unique needs and long-term goals. Ensure the chosen system meets your current needs and can adapt to future healthcare rules, technological advances, and evolving patient care needs. By selecting a vendor that is a true partner in your EHR migration journey, you can get the most out of your investment and achieve the outcomes you want for your organization and patients.
Customization and Flexibility
Assessing Customization Needs
During the EHR migration process, you need to check what your health organization needs to personalize. This lets you change the EHR system to go with certain ways of working, documents needed, and what users like.
Think about these things:
- Clinical Workflows: Start with a deep examination to see certain clinic routines. They might need backing from the Electronic Health Record (EHR) system. By moving templates, forms, and clinical decision help tools, healthcare workers can raise how efficient and correct they are in the patient care process.
- Reporting Requirements: Then, it’s important to outline the certain reports and analytics necessary for improving quality and complying with rules, and for improved operations. With customizable reporting in the EHR, healthcare experts can use EHR data and make informed decisions.
- User Preferences: Lastly, actively involve end-users in this customization journey to ensure their specific needs and likes are met. By setting up personalized dashboards and user-friendly interfaces, users are happier and this leads to more use of the system in your healthcare organization.
Ensuring System Flexibility and Scalability
A good EHR system needs to adjust and grow easily as your organization evolves. Think about these details during EHR migration:
- Modular Design: When selecting an EHR system, opt for one with a modular design that allows seamless addition or removal of functionalities based on specific needs. his means you can add or take away parts based on what you need. This way, your system can quickly adapt to changes in the doctor’s office and new rules easily.
- Scalability: Make sure your EHR system can grow with you. Whether you’re adding new offices, seeing more patients, or offering new services, your system needs to handle more information and users without slowing down. This helps keep everything running smoothly.
- Integration Capabilities: Pick an EHR system that works well with new technology and healthcare IT breakthroughs. This ability means your system can keep up with changes in how healthcare is done. This helps your organization do its best and stay competitive in a fast-changing healthcare world.
By thoughtfully weighing choices, identifying specific personalizations, and affirming that the system is elastic and expandable, you can select the EHR system that bolsters a smooth EHR migration and boosts your organization’s quality of care.
3. Preparing and Transferring Data
Healthcare Data Archiving Solutions
Healthcare data archiving solutions are crucial because EHR systems produce vast amounts of data. Archiving preserves old patient information, making sure it’s both secure and easy to find. Also, it meets all legal standards.
Hospitals and clinics need these strategies to maintain data integrity, reduce storage costs, and improve data retrieval efficiency.
Solid healthcare data archiving solutions mean that vital patient details are saved and ready when needed, ultimately leading to better care for patients and smoother operations.
EHR Data Migration Challenges
Moving to a new Electronic Health Record (EHR) system isn’t always easy and can come with EHR data migration challenges. It’s better to spot problems early for a smoother changeover. Two main obstacles are data compatibility and data loss risks during EHR migration.
Data compatibility means ensuring data from the old system works with the new one. This can be tricky as different EHR systems use different ways to save and transfer data. Strong data mapping and changes during EHR migration can tackle this.
We can’t ignore the data loss risks either. Losing important patient information can harm patient care and lead to legal issues. Solid backup plans and checks can mitigate these risks during EHR migration and ensure no crucial info is lost when moving data.
Also, moving large amounts of data can be tough and slow during EHR migration. It could lead to more mistakes and delays. Using good data moving tools, detailed planning, and step-by-step moving plans can make this less difficult during EHR migration.
Facing these challenges head-on with smart methods and modern tech can lead to an efficient and effective EHR data migration. By doing this, the overall performance and efficiency of the healthcare system can get improve.
Taking on these challenges directly, applying top methods, and using new tech can help create a successful EHR data migration. This progress then boosts the healthcare system’s total efficiency and performance during EHR migration.
Data Cleaning and Validation
Importance of Data Quality in EHR Migration
High-quality data is key to your EHR migration success. Clear and correct data boosts patient care and makes healthcare processes smoother. Also, it helps healthcare pros make better decisions. But, faulty information can do lots of harm during EHR migration. Mistakes, delays, and even risks to patient safety can occur.
So, the first important step in preparing data for EHR migration is to make sure your data is clean and validated. This preparation paves the way for an easy shift to your new system.
Steps for Data Cleaning
- Data Standardization: Keep things similar in healthcare data systems, it’s key for EHR migration. The date styles, measurements, and medical terms should all match.
For example, swap between metric and imperial or use common medical codes like ICD-10 or SNOMED CT. This balance makes joining the dots easier and speeds up research across different healthcare IT systems during EHR migration. Also, it speeds up data sharing and helps patients.
- Duplicate Removal: Use smart tactics and formulas to spot any double records in electronic health records (EHRs) during EHR migration. Healthcare people can get rid of repetitive info to keep the EHRs neat and help put all data in one place. It lowers the chance of mix-ups, making data better and the system faster during EHR migration.
- Accuracy Checks: Serious checks are needed to be sure of the data in healthcare records. Double-check patient info, like names, addresses, and past health history using sources you can trust. This helps spot and fix mistakes quick during EHR migration. Being careful with these details keeps data in check and cuts down on false info or medical slip-ups during EHR migration.
- Completeness: Aiming to fill in every detail is important to keep patient records up to date in the new EHR system during EHR migration. Double-checking that all necessary fields are correct and filled out is vital for smooth team-work and smart clinical choices during EHR migration. Quickly dealing with any errors or empty information is crucial for seamless patient care and to get the most out of the EHR system during EHR migration – for doctors and patients.
Data Validation Techniques
- Automated Validation: Employ automation to inspect data for errors, precision, and fullness. This auto-check quickly spots irregularities that must be fixed ahead of EHR migration.
- Manual Review: Carry out a manual inspection of vital data parts to make sure they hit the quality bar. This requires double-checking with original files and asking health workers to confirm. This is important when in the process of EHR migration.
- Pilot Testing: Try a small-scale test run with a portion of data to check if the EHR migration process works. This finds potential problems and leaves room for adjustments prior to a large-scale EHR migration.
Data Mapping
Understanding Data Mapping in EHR Migration
Data mapping is all about connecting information from the old Electronic Health Record (EHR) system to the right spots in the new system. It ensures that every bit of needed info lands in its proper place during EHR migration.
Let’s walk through the steps.
Steps for Effective Data Mapping
- Identify Data Elements: First, list every key data detail required for EHR migration. Think patient info like names, ages, contact info; diagnoses, medications, and allergies; things like treatment procedures and prescriptions; as well as insurance and payment details.
- Define Mapping Rules: Next up, map out rules for moving each data point from the old system to the new one. This step means deciding on any changes in data, pinpointing any formatting changes to make during EHR migration, and noting any processes for normalizing data.
- Use Mapping Tools: With the rules set, it’s time to use data mapping tools. These specialized tools speed up the process by doing the heavy lifting for you. They keep data straight during EHR migration, lowering the risk of mess-ups.
- Validate Mapping: Lastly, prior to the actual EHR migration, check the mapping rules thoroughly. This step checks that every data point ends up where it should and is understood by the new EHR system, lowering the risk of losing or misplacing data.
Secure Data Transfer
Ensuring Data Security During EHR Migration
Keeping data safe during EHR migration is important. Because health information is so private, it’s vital to protect it against unwarranted access, leaks, and damage.
Firms can uphold data’s secrecy, wholeness, and access during the EHR migration by using solid safety rules, like cyphering, using many authentication steps, and regular safety checks.
This not only keeps patient information private but also keeps stakeholders trusting the healthcare system, making a dependable and secure environment for managing private health data.
Secure Transfer Protocols
- Encryption: Encrypt the data both in transit and at rest to ensure its safety from unwarranted access. This process guarantees that any intercepted data during EHR migration remains unreadable without the correct decryption keys.
- Secure Transfer Channels: Employ safe transfer channels, like Secure File Transfer Protocol (SFTP) or Virtual Private Networks (VPN), to transmit data safely between systems during EHR migration.
- Access Controls: Put in place strict access restrictions to limit who can see and move data during EHR migration. Make sure to permit only authorized people access to private information.
Monitoring and Auditing
- Real-Time Monitoring: Keep track of sharing activities in real time. This helps spot any activities events during EHR migration.
- Audit Trails: Keep a close eye on every action taken during data transfer. Audit logs not only show who’s looked at the data, but also what they did, creating a clear trail for the EHR migration.
By preparing and shifting info carefully, through in-depth cleaning processes, strict validation assessments, thorough mapping methods, and sticking to safe transfer rules, a successful and protected EHR migration is possible.
This careful method not only looks after the data’s wholeness but also is vital in boosting quality patient care. It does this by guaranteeing correct and dependable info sharing within healthcare systems.
EHR Data Migration Services Certification
Having an EHR data migration services certification is really important. It helps us stick to the industry rules, keep the data safe, and shows that the service is good and dependable.
EHR data migration services that are certified minimize errors and keep sensitive information safe. They use strong encryption, secure ways to send data, and strict access controls to keep data safe during the move.
Certifications like HITRUST CSF, ISO 27001, and SOC 2 Type II show that the service provider meets high levels and provides dependable services. This makes for a safe and smooth EHR migration.
4. Staff Training and Change Management
Training Programs
Importance of Training in EHR Migration
Staff training is crucial for a successful EHR migration. When everyone knows how to use the new system, it can run smoothly with fewer issues. Thorough training prepares healthcare workers and office staff, enabling them to learn and use new features and procedures with ease.
This smooth change-over to the new EHR makes the system easier to adopt. Also, it leads to better patient care and more efficient operations.
Developing a Training Curriculum
- Needs Assessment: Start with a total examination of training needs. Find out what skills your team lacks. This will make your training more spot on and helpful for all.
- Role-Based Training: Custom training materials should be different for each role in your organization. Think of unique guides for doctors, nurses, administrators, and IT staff. Each group’s focus during the EHR migration might be different, and specific training helps everyone understand better
- Hands-On Training: Boost your training with interactive pieces. Let users practice with the new EHR system in a safe setting. This hands-on approach is key to growing confidence, skill, and familiarity with the system. Smoothens eventual adoption and use.
- Ongoing Support: Plan for regular training and help to handle any queries or issues post EHR migration. Offer recap courses, high-level training, and resource access. This will keep staff updated on new system features and industry norms. By giving continuous help, your team will be able to fully utilize the EHR system and meet changing needs effectively.
User Adoption Strategies
Promoting User Adoption During EHR Migration
Getting people to use Electronic Health Record (EHR) systems is key to a successful switch. Getting the team on board is key in taking full advantage of the new EHR system. One way for healthcare organizations to do this is by using custom strategies to involve their staff and improve their skills. The goal is to help everyone get the most out of the EHR system. Here’s how:
Strategies for Enhancing User Adoption
- Engagement and Communication: Keep your staff in the loop about why EHR migration is a great idea. Discuss how it can better patient care, organize tasks easily, and cut down on paperwork.
- Involve Users Early: The best game plans come from team input. Ask what your staff think about the EHR migration. Their ideas could be useful, but it can also help everyone feel more connected to the change.
- Champions and Super-Users: Look for your EHR experts in each department. They can speak up for the EHR system and support their colleagues. They will help solve problems and ensure the EHR migration goes well.
- Feedback Mechanisms: Having a place where people can voice their opinions about the change is crucial. An ongoing conversation allows for changes to be made when needed, making the EHR migration better and increasing the chance for everyone to get on board.
Managing Resistance to Change
Understanding Resistance in EHR Migration
When switching to Electronic Health Record (EHR) systems, change resistance is a common hurdle. Staff might be uneasy about learning new systems. They might be afraid that their routines will get disrupted. Or maybe, they just doubt the benefits of EHR migration.
Therefore, careful planning of change management strategies is crucial. With it, we can tackle this resistance efficiently in healthcare situations.
Strategies for Managing Resistance
- Transparency and Communication: During the EHR migration, keeping communication transparent and regular is important. Staff needs frequent updates about why the switch is happening, the expected benefits of the new EHR system, and a well-defined plan for introducing it. This calms uncertainties and sets the right expectations.
- Addressing Concerns: Properly listen to what the staff is worried about and address those worries quickly for a good EHR migration. Clear answers and solutions to raised problems can ease worries and build trust, helping with a smooth EHR migration.
- Incentivizing Adoption: Motivate and encourage staff to take part in the EHR migration. Reward and recognize early adopters and engaged participants. This creates a positive atmosphere, inspiring others to join in.
- Providing Support: Ample support during the change phase is critical. Establish help centers, have tech-savvy IT help on call, and offer guides like user handbooks and helpful FAQ’s to guide staff through the new EHR system effectively.
Leadership and Change Management
- Leadership Involvement: Leaders from all levels should support and actively promote the EHR migration plan. This includes top executives, department heads, and team leaders. Their role is crucial in setting the tone for change. Their duty is to provide a clear vision, align it with the organization’s aims, and provide the needed resources for a smooth EHR migration.
- Change Management Plan: You need a complete change management plan. This must not just lay out the steps, times, and roles. It also needs deep analyses of stakeholders. Identify key people and organizations impacted by the EHR migration and make the communication, training, and support to match their needs. Always look for feedback to tailor the plan, cultivating engagement and a sense of ownership.
- Monitoring and Adjustment: Set up tough tracking that notes huge factors related to EHR migration progress. Check these measures often to see how well the EHR migration plan is working out and find spots to get better at. Be ready to tweak in real-time centering around unfolding challenges or chances to make the change smoother. By staying flexible and quick to respond, the organization can bend with changing situations and get the EHR migration done without a hitch.
In shaping and rolling out detailed training plans for different user groups, energetically encouraging user participation through workshops and individual support meetings, and dealing directly with any pushback by offering clear info, constant learning, and ways to share feedback, you can nicely guide a smooth EHR migration.
This move doesn’t just raise your healthcare group’s speed and success; it also guarantees a smooth blend of the new program into everyday work, pushing patient care results and overall organization performance to new levels.
5. Testing and Go-Live
Pre-Go-Live Testing
Importance of Testing in EHR Migration
It’s important to carefully test during an EHR migration. Thorough testing helps identify possible problems, checks how the system works, and makes sure the new EHR matches your healthcare organization’s needs.
If you test like a professional, you can dodge issues like system downtime, incorrect data, and workflow disruptions. If you don’t test right or race through it, these problems could harm your patient care quality.
Steps for Pre-Go-Live Testing
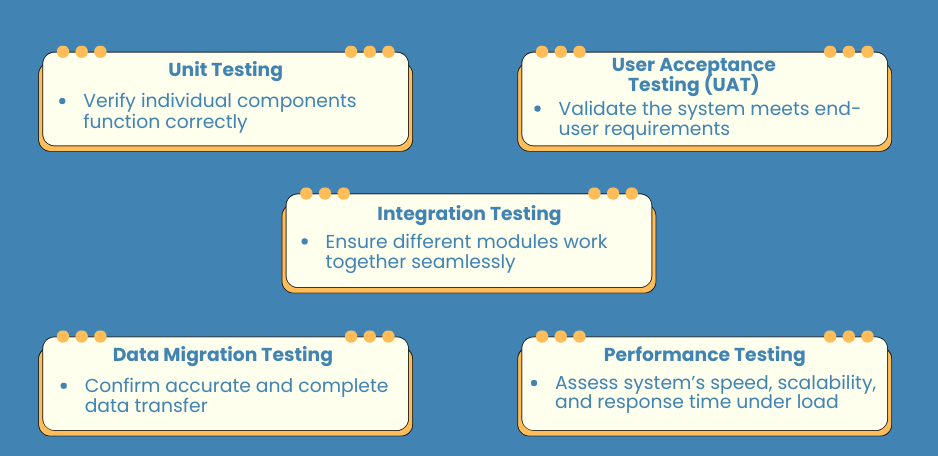
- Unit Testing: Simply put, unit testing means making sure each EHR system part works right. This means checking particular features and functions to see if they’re doing their job.
- Integration Testing: This process checks how well different EHR system parts work together. It’s vital for making sure the system can work with other health IT systems, like lab info systems and pharmacy systems, during the EHR migration.
- User Acceptance Testing (UAT): Here we get end users to tell if the EHR system does what they need it to. UAT spots any user issues and makes certain the system fits clinical workflows well.
- Data Migration Testing: This test makes sure all the data is moved right from the old system to the new EHR migration one. It checks that data mapping rules are applied right and no important info got lost during the EHR migration.
- Performance Testing: Here we put the EHR migration system under performance testing to see how it holds up. We’re looking at response times, scalability, and overall performance under different load conditions. The idea is to be certain the system can cope with busy times without performance dropping.
Go-Live Support
Strategies for a Successful Go-Live During EHR Migration
When the new EHR system is ready to go into action, it’s a big occasion. It means all the hard work is about to pay off. But, it needs careful thought and lots of support to make sure everything runs smoothly. Good go-live support is vital so we steer clear of problems, fix issues quickly, and help people get used to the new system. What does this support involve? Here’s what we need:
Key Elements of Go-Live Support
- Go-Live Planning: First, we have to make sure we have a solid plan when the EHR migration takes over. This plan has to list out all the steps one by one, accompanied by a detailed timeline. Next, we have to know who is responsible for what, every step of the way. Additionally, we need a backup plan, just in case anything unexpected comes up. That keeps everything running as it should.
- Support Teams: A special team is needed during the go-live phase. This team is made of IT experts, people who know all about EHR migration, and super-users who have a lot of experience. Their job? Sorting out any tech problems, and offering fast, on-the-spot help to all users. This makes sure everyone moves to the new system without any hiccups.
- Communication Channels: Transparent communication channels are key when it comes to resolving issues fast during the start phase. Support desks, hotline services, and web-based help sites make it easy for folks to report problems swiftly and get them sorted. This paves the way for a smoother EHR migration.
- Training Refresher Sessions: Providing top-up training sessions helps drive home key points and answers staff questions. With everyone feeling ready and confident, companies can help their teams adjust more easily, for a successful EHR migration.
- Gradual Rollout: It’s worth thinking about deploying the new EHR migration step-by-step. This means introducing it to different departments or locations in stages. By making changes bit by bit, it reduces disturbances, handles potential obstacles, and levels out the chance of big problems. In turn, this offers a smooth EHR migration.
Post-Go-Live Evaluation
Assessing the Success of EHR Migration
Evaluating after going live is key to realizing how well the EHR migration went and what might need a tune-up. This stage means keeping an eye on system functionality, garnering user opinions, and adjusting as needed to make the new EHR system top-notch. Let’s take a look at the post-live evaluation.
Steps for Post-Go-Live Evaluation
- Performance Monitoring: Keep a close watch on the workings of the fresh Electronic Health Records (EHR) system for non-stop top-tier operation. Look out for things like:
- System uptime: Make sure the system is available and operational at all times.
- Response times: Track how quickly the system responds to user inputs.
- Error rates: Monitor the frequency of errors that arise during use.
- User Feedback Collection: Get thoughts from those using the system to deeply understand their experience with the new EHR migration set-up. Use different ways to gather user thoughts, like surveys, group discussions, and chats, to learn what difficulties users have and where the system can do better. Daily understanding of these user views is pivotal to tailoring the EHR migration system to meet the many needs of professionals in healthcare and better overall user contentment.
- Issue Resolution: Fix problems promptly that users find to make the EHR migration process smooth. Make necessary changes to fix system errors, make it easier to use, and make users happy during the switch. By sorting out user issues quickly, health organizations can earn users’ trust and make their experience with the new system good.
- Data Quality Audits: Regularly check the data for quality to be sure it’s accurate, complete, and consistent in the new EHR system. Find and deal with discrepancies or errors found during checks to keep the data reliable. Regular data checks are crucial to keep the EHR system correct and back up good patient care.
- Continuous Improvement: Encourage a never-stop-improving mindset in the organization by often looking at the EHR system and making updates based on user feedback and changing healthcare needs. This covers adding new things, streamlining workflows, and continuous training and support for users. By celebrating continuous improvement, health organizations can respond to changing needs, make the system easier to use, and give better care to patients.
Through detailed testing before launch, solid support during the transition, and full assessments after go-live, your EHR migration can be a success. This improves your healthcare group’s productivity and effectiveness.
6. Post-Migration Optimization
System Optimization
Importance of Optimizing the EHR System Post-Migration
After moving to an Electronic Health Record (EHR) system, the next step is to adjust it for best use.
Fine-tuning the EHR involves changes that boost its efficiency and support for clinical workflows, ultimately improving patient care.
By focusing on system optimization after the EHR migration, healthcare providers can improve their operations and processes, thus upgrading patient care quality.
If they don’t prioritize optimization after the migration, the system might not perform at peak levels, causing delays in efficiency and quality improvements.
Key Areas of System Optimization
- Workflow Customization: Make the EHR system fit with your unique healthcare flow. You can change templates, forms, and orders to suit different departments.
- System Performance Tuning: Enhance the system’s speed and reliability by adjusting server settings, database details, and your network. Quick response times are important for accessing patient data during and after EHR migration.
- Interface Enhancements: Enhance the EHR system’s look for easier use and quicker learning for staff. This can mean making navigation simple, cutting down clicks for basic tasks, or customizing dashboards to display relevant information.
- Integration with Other Systems: Integrate the EHR system well with other health systems like lab information ones, radiology ones, and billing software. Integration ensures data flow and working together, vital for a successful EHR migration.
Ongoing Training
Continuous Training for Sustained EHR Migration Success
Keeping your team skilled is key to making sure your health care organization and its EHR system are in sync. Always training bridges the gap in understanding, keeps everyone up-to-date, and encourages the use of new strategies and features brought into the EHR system after the EHR migration.
Strategies for Effective Ongoing Training
- Regular Training Sessions: Scheduling frequent training sessions, every week or two, benefits staff. These sessions allow them to easily understand the functions of the new system.
- E-Learning Modules: Building a broad library of e-learning modules gives staff a big advantage. It means they can access training whenever it suits them. These web-based resources offer independence and adaptability, letting staff learn as they go and fitting into their packed timetables.
- Role-Based Training: It boosts the learning experience to give specialized lessons, each suiting the unique tasks different team members handle. This focused method ensures every user bunch gets custom and pertinent learning in line with their certain roles, boosting their expertise in using the EHR system effectively.
- Mentorship Programs: Setting up structured mentorship programs can help a lot after an EHR migration. Experienced users help guide new and struggling staff. This support creates a team learning space, making knowledge transfer easy and speeding up system adoption. This whole process helps make the EHR migration a win.
- Feedback-Driven Training: Keeping a strong feedback system in place is key to endlessly improving the training after you start a new EHR. Feedback highlights areas that might need more training or adjustments. Using this input in your plan makes you effective at solving issues, refining training, and supports the staff through and beyond the EHR migration period.
Continuous Improvement
The Role of Continuous Improvement in EHR Migration
Continuous improvement is not just good, it’s actually a must for keeping Electronic Health Record (EHR) upgrades on track in health groups. These groups need strong plans for regular checks and tweaks of their EHR systems.
This keeps everything up to date with new tech, changing rules, and fresh medical methods. Sticking to making things better all the time lets health providers make sure their EHR systems are really helpful. This helps them give excellent patient care easily and stay leading the way in health innovation.
Steps for Continuous Improvement
- Performance Monitoring: Set up a continuous tracking program to follow key factors such as;
- How often the system works without pause.
- How quick the response is.
- How happy the users are.
Use these facts to spot areas to make better and to see the change in results after EHR migration.
- User Feedback Integration: Always gather and study comments from users to grasp their experiences and problems with the EHR system. Use these comments to sort out which enhancements to take care of first and address any issues that come up after EHR migration.
- System Updates and Upgrades: Keep up with the newest updates and improvements offered by the EHR provider. Updating the EHR system regularly makes sure it has the newest features, security fixes, and better performance capabilities.
- Process Optimization: Keep checking and fine-tuning both patient care and office procedures to make full use of the EHR system. This includes making workflows smoother, cutting out repeated tasks, and getting rid of methods that don’t work well during and after the EHR migration.
- Innovation and Best Practices: Driven to keep learning about the latest trends, best methods, and new ideas in health IT. Bring in new technologies and ways that can better the usefulness and success of your system after EHR migration.
Healthcare organizations can ensure their Electronic Health Record (EHR) updates exceed expectations. How? By focusing on system optimization, offering regular training, and encouraging continuous improvement. These efforts are vital. They make sure that after the EHR migration, the upgraded EHR system works well. This system not only makes patient care processes more efficient, it helps provide better patient care.
Also, these steps keep the EHR system flexible. It stays quickly responsive to the changing health industry, setting organizations up for future success and innovation.
7. Measuring Success and ROI
Key Performance Indicators (KPIs)
Importance of KPIs in EHR Migration
Want to know if your EHR migration is working? You need to watch certain signs, or key performance indicators (KPIs). They’re like an evaluation report for your new system – they show how well it’s helping your organization.
KPIs are just numbers, yes. But they help you find out if your EHR migration is doing what you need it to. Some KPIs you should keep an eye on include how well the new system aids clinical work processes, betters patient care, and boosts operations. Let’s break down these essential KPIs.
Essential KPIs for EHR Migration
- System Uptime: System uptime is an important indicator of the reliability of your EHR system. Higher uptime means fewer issues, ensuring patient data is always accessible, which is essential for a smooth EHR migration.
- User Adoption Rates: This shows how many people on your team are using the new EHR. If more staff use it, your EHR migration is likely successful. Plus, it shows your training is working.
- Clinical Productivity: Look at key daily numbers, like how many patients are seen, the time taken for paperwork, how smooth your work process is. If these improve after the EHR migration, then you know it’s helping your workflow.
- Data Accuracy and Completeness: Assess the precision and thoroughness of information keyed into the EHR program. Reliable, full data is crucial for making clinical choices and signifies a victorious EHR migration.
- Patient Satisfaction Scores: Gather comments from patients on how they found the healthcare services. Better scores for patient satisfaction could be a straight-on impact of better procedures and communication provided by the EHR migration.
Financial Metrics
Assessing Financial Impact of EHR Migration
Looking at how EHR migration impacts your bottom line is key to finding out its return on investment (ROI). Money-based metrics offer a glimpse into cost reductions, revenue boosts, and overall financial improvement from the new EHR system. By studying these metrics, medical institutions can weigh the financial worth of their EHR migration work.
Key Financial Metrics for EHR Migration
- Implementation Costs: When taking on the task of EHR migration, it’s key to track all potential costs associated with it. These can be software licenses, hardware upgrades, staff training and fees for external specialists. Understanding these expenses helps in planning your budget and figuring out the ROI of your EHR project.
- Operational Cost Savings: The effectiveness of EHR migration in curbing daily costs comes down to examining how much money we save by ditching old paper-based work routines. This could mean using less paper, having fewer transcription bills, or spending less on office management. Switching to digital records helps healthcare centers simplify their work, cutting costs in the long run.
- Revenue Cycle Improvement: Checking up on the betterment of the income cycle after EHR migration is key to see how financially efficient the system is. Signs of improvement might be speedier billing, fewer rejected claims, and a jump in collection productivity. A properly set up EHR system is hoped to smooth out the income cycle, underlining a successful switch and upgraded operations.
- Return on Investment (ROI): ROI calculation involves measuring the financial gains from EHR migration against the start-up costs. A positive ROI means the electronic system’s benefits surpass the transition costs. Such financial assessment highlights the cost-effectiveness and lasting benefits of choosing an EHR solution.
- Productivity Gains: EHR implementation can lead to financial gains through improved clinical productivity and efficiency. By measuring enhancements in patient flow, slashed appointment wait times and better use of resources, healthcare providers can see real improvements in daily operations. Increased productivity doesn’t only improve patient care but also promotes economical healthcare delivery.
Qualitative Benefits
Evaluating Qualitative Benefits of EHR Migration
Alongside quantitative metrics, looking into the quality gains of EHR migration provides a full picture of its effect. Quality gains cover boosts in patient care, worker happiness, and the overall performance of the organization. While these gains might be tough to measure, they are key to understanding the overall success of EHR migration.
Key Qualitative Benefits for EHR Migration
- Enhanced Patient Care: It’s essential to identify the improvements in patient care quality from EHR migration, including better coordination of care, timely access to patient files, and fewer medical errors. Improved patient care is an important benefit that successful EHR migration can provide to medical facilities.
- Staff Satisfaction: Gathering feedback from healthcare providers and administrative staff is precious to understanding how the new system works after the EHR migration. By assessing their satisfaction levels, organizations can dictate if the system fits their workflows, possibly lowering work-related stress. If the workers are happier, it’s often an indication that the EHR system supports their roles efficiently, leading to a more effective healthcare setting.
- Improved Communication: Evaluating EHR migration isn’t just about technology; it’s about people too. It’s key to see how the change impacts team communication. The new setup could help health teams work better together and improve their care decision making. This is a big plus for patient care.
- Regulatory Compliance: EHR systems need to meet legal and standards reporting needs. Post-migration is a good time to check the system makes this easier. If it helps with paperwork and standards, that’s a win for data safety and workflow.
- Innovation and Adaptability: Healthcare is always growing, and the EHR system needs to keep pace. Does it welcome new tech and better ways of working? An adaptable EHR system helps future-proof hospitals and brings lasting benefits from the EHR migration.
Healthcare organizations can accurately gauge the success and payoff of their EHR migration by continuously keeping an eye on major performance pointers, economic figures, and plus points that aren’t just about numbers.
These careful checks don’t just assign a number value to the benefits obtained from the EHR system start-up. They also show how big the system’s role has been in bettering patient care results, and how well it fits with bigger organizational aims.
How Virtelligence Can Help with EHR Migration
At Virtelligence, our skilled team provides tailored services to ease your EHR migration, warranting a seamless shift and improved operation efficiency.
Expertise and Customized Solutions
We recognize the unique demands of each healthcare system, so we offer customized solutions tailored to these specific needs. Our consultants are thoroughly screened, well-informed, and experienced in EHR migration, ensuring your organization benefits from top-quality talent.
We prioritize minimizing pause time, cost management and strengthening data protection throughout the move process. If enhancing your EHR migration is your goal, Virtelligence is ready to assist.
Head to Virtelligence to discover more about how we can support your organization in every phase of the EHR migration.
EHR Data Migration Services Careers
Final Thoughts
Recap of Key Points
Boosting your EHR migration needs careful thought and action at every step. Let’s review the main areas we discussed:
- Introduction and Overview: Understanding why EHRs matter and why to shift to a more developed system.
- Planning Your EHR Migration: Initial checks, setting goals that stand clear, bringing in crucial players for a solid base.
- Choosing the Right EHR System: Evaluating choices, evaluating customization requirements, ensuring system adaptability and growth capacity.
- Preparing and Transferring Data: Watching over data standards through cleaning, validation, mapping, and secure shift procedures.
- Staff Training and Change Management: Setting up valuable tutorials, boosting user adoption, and controlling reluctance to change.
- Testing and Go-Live: Complete pre-launch tests, round-the-clock launch support, and an exhaustive post-launch review.
- Post-Migration Optimization: Giving attention to system enhancement, continuing tutorials, and non-stop improvement to fully use the new EHR system.
- Measuring Success and ROI: Observing major performance pointers, financial criteria, and qualitative gains to assess the success of the EHR migration.
Adopting the key steps in this guide, healthcare organizations can confidently tackle the challenges of EHR migration. A well-led EHR migration boosts not just the speed and success of clinical processes, but elevates patient care and drives organization-wide goals.
Keep in mind, the journey isn’t finished at the launch. Regular check-ups, support, and fine-tuning are imperative to uphold a top-tier EHR system that shifts to meet your health institution’s changing demands.
Dive into the process, engage your team, and remain dedicated to giving your patients the best results. To get more help with your EHR migration needs, contact us at Virtelligence.
Our experienced team is on standby to provide customized solutions and assistance to guarantee your EHR migration is successful. We appreciate your time in reading this guide. We trust it offers helpful knowledge and handy approaches to support a triumphant EHR migration.
FAQs
What is optimization in EHR?
Optimization in EHR includes sharpening and amplifying the electronic health record system for better performance, ease of use, and overall impact.
This includes tailoring flows to simplify tasks, boosting user interfaces for effective usage, tying in smoothly with additional health IT systems for full-scale patient care, and keeping updates ongoing to match current methods and regulatory standards.
By adjusting the EHR details, medical providers can better the patient care process, data handling, and total working efficiency.
What is EHR migration?
EHR migration, short for Electronic Health Record migration, is a carefully crafted process of moving digital health records from one system to another.
This involves careful planning, rigorous data scrubbing to ensure precision, comprehensive data mapping for maintaining integrity, security measures for the safe data transfer, and thorough testing to make sure all patient data is transferred correctly and securely to the new system.
This process ensures the privacy and integrity of sensitive medical data throughout the EHR migration.
Are there any strategies or best practices to ensure that the EHR system supports patient-centered care?
Yes, there are multiple ways to make the Electronic Health Record (EHR) system better to support patient-centered care.
- One, make user-friendly interfaces. This means designing EHR interfaces that are simple and easy for healthcare providers to understand and use. This helps them work more effectively, which leads to higher quality care for patients.
- Two, make it interoperable. A good EHR system should be able to share data with other health IT systems without any trouble. This makes it easier for healthcare providers to share patient information and improves patient outcomes.
- Three, make it customizable. The EHR system should be adjustable for specific clinical needs and rules. This lets healthcare providers arrange their workflow, record correct data, and alter the system to accommodate their specific practice needs.
- Last, give patients access. Patients should be able to look at their health records and talk with their healthcare providers. This encourages patient engagement and shared decision-making. By enabling ways for patients to access their health records securely and conveniently, patients can take an active role in their care. This leads to better health results and happier patients.
How to transfer data from one EHR to another?
It’s easier when you do it step by step.
- First comes data cleaning. Make your data uniform, remove any double entries, and fix any mistakes. This way, your data stays accurate and can be relied upon.
- Next, you’ll want to do data mapping. Identify matching data fields between the outgoing and incoming systems. This helps create links and guarantees no information gets lost during the EHR migration.
- Secure transfer is next. Make sure you’re using strong encryption options and secure protocols like SSL/TLS for the data shifting process. This prevents unauthorized peeks and meddling.
- After switching over, like checking your work in a math test, it’s time for Validation. You’ll want to confirm that all transferred data remains intact, complete, and error-free. Automated checks and human review will make sure this happens.
- Lastly, don’t forget testing. Ensure that the new system and switched data are getting along, with features functioning properly, smooth operation, and end-users happy. A thorough test will ensure the transition’s success. And that’s all it takes.
What is the step-by-step process for implementing an EHR?
Here’s how to implement EHR, step by step.
- Planning: Look at what you need, decide your goals, and budget.
- Selection: Find and select the best EHR system for you.
- Preparation: Cleanse, organize, and confirm data for EHR migration.
- Training: Teach your staff and involve stakeholders.
- Testing: Perform detailed testing before going live.
- Go-Live: Stick to your go-live plan and have support teams ready.
- Optimization: Keep improving and training even after launch.
How is data extracted from EHR?
We pull out information from EHR in many ways, for instance:
- Database Queries: SQL queries help us grab the right data.
- APIs: This involves using coding interfaces given by the EHR company.
- Export Tools: These are tools built into the EHR system to help with this.
- ETL Tools: These tools help collect and move data during EHR migration.
How do you transfer data between systems?
There are several steps.
- Data Mapping: This means making sure data fields in the original and new systems match.
- Transformation: This is when we change data into the needed formats for EHR migration.
- Secure Transfer: Here, we use safe methods like SFTP or VPN.
- Verification: It’s all about cross-checking the data transferred during EHR migration.
- Validation: This involves tests to confirm data accuracy and completeness.
What is data conversion in EHR?
Electronic Health Records (EHR) often encounter a tricky step: data conversion. Data is moved from its old format to a new one that fits the updated EHR system. This careful change makes sure no patient detail gets lost and aligns with the stages of EHR migration. Also, it smoothly adds each piece of data into the new system. It keeps things tidy, exact, and easy to use for both doctors and patients.
What is interoperability between EHRs?
Interoperability the power of different EHR systems to flawlessly exchange, understand, and use data, often an important part of EHR migration. This lets patient info be spread across varied healthcare providers and IT systems, improving care teamwork and patient results. Interoperability helps data move smoothly between EHR platforms. This is vital in giving caregivers total, current patient facts to guide diagnosis and treatment choices.
What is EHR connectivity?
In health tech lingo, it’s the smooth joining of Electronic Health Record (EHR) systems with other health IT systems and gadgets. The ongoing, real-time info swapping between diverse healthcare players is enabled. This exchange, initiated by EHR connectivity, smoothes out workflow. It encourages teamwork among healthcare pros, and aids in making more informed clinical decisions during and after EHR migration.