
Barriers! Hectic Processes! Compliance chaos! Yes, we understand. Quality healthcare documentation is crucial yet challenging in today’s complex medical landscape. While technology has streamlined record-keeping, barriers remain that hinder effective patient care.
This article examines opportunities to simplify documentation through collaboration, communication, and continual improvement. It explores how assessing current processes, minimizing shorthand, leveraging speech recognition, and selecting the right developed custom application that can optimize workflows.
Why Is Documentation Important In Healthcare?
Documenting a patient’s medical records is not just about writing down what happened during the visit but also includes other steps to increase the overall quality of care. More importantly, healthcare documentation maintains a collaboration of information to be passed on through providers or to specialists.
Medical transcriptionists encompass a wealth of patient health data, including previous and current conditions and information on the patient treatment process. Ultimately, precise healthcare documentation can comprehensively and accurately provide a picture of the patient’s medical history.
Understanding the Importance of Accurate and Efficient Healthcare Documentation
One of the fundamentals of healthcare is documentation. Traditionally, healthcare practitioners are saddled with an ocean of paperwork, which points out a huge issue for the whole industry, managing information effectively and accurately. Inaccuracies in healthcare documentation can give rise to incorrect treatment procedures, billing problems, or, at worst, patient injuries.
It’s a high-pressure zone where every word is crucial. Healthcare documentation plays a significant role in administrative workload, which is implicated in physicians’ burnout. Studies show that doctors spend more time documenting than with patients.
Incomplete or misleading healthcare documentation can bring life-threatening problems for the patients and the safety of the whole healthcare system. For example, an incorrect chart, whose content shows a patient’s allergy, could be fatal for them. Inappropriate medical history or medication lists challenge treatment or intervention success.
What Is Effective Healthcare Documentation?
Giving precise information about the patient is crucial to ensure the best healthcare. The oversight problem in healthcare documentation causes both internal and external reports to be inaccurate. This diminishes the quality of patient healthcare.
Precise healthcare documentation serves as the repository for every detail of patient care. When executed properly, this contributes to the patient’s expedited recovery. Accurate information collection will help the provider avoid legal disputes. On the other hand, it also leads to the specialist’s competence and indicates credibility that the provider respects the importance of proper record-keeping.
Key Factors For Healthcare Documentation Improvement
Here are some key factors of effective healthcare documentation include:
- Provide factual, consistent, and accurate input
- Update the information after any recordable event
- Make sure all information is current
- Confirm that all entries are legible and signed
- Avoid meaningless jargon, phrases, or abbreviations that aren’t commonly understood
How Can Healthcare Documentation Be Improved?
1. Assess Communication
As to the improvement of healthcare documentation, providers must record all those significant details. Additionally, it is necessary to eliminate any uncertainty in the comprehension of the documentation from its creators to its users. Even if physicians can document crucial facts, it will be meaningless if the questions remain unanswered.
2. Reduce Shorthand
Among the foremost results of evaluation communication between those groups is finding out how and where misunderstandings happen. This miscommunication might appear as shorthand, which is unclear because the patients don’t know.
It may not be clear and even inaccurate with shorthand because this is only the case if both parties can recognize and have the same meaning with the shorthand they use.
3. Utilize Speech Recognition
On some days, due to the time-consuming nature of documentation, a pile-up of incomplete documentation is done, and working through the stack of papers has now become the daily call of the day.
The results are errors or inconsistencies in the documentation, but the physician’s time is taken away. With speech recognition, doctors can simply dictate their notes rather than type them, which makes the entire process much faster.
4. Select the eMR platform
During their activities, doctors perform routine clerical and administrative tasks, but the best thing you can do to optimize the time spent on these tasks is to use the right EMR tools for your organization. Unfortunately, it is not a secret that some EMRs are easier to use than others.
5. Educate your team
There may be decreased productivity because of poorly updated, inaccurate, or inadequate documentation; therefore, your team may require education. Ensuring your team knows documentation well; for others, it’s necessary to revisit the foundation. The results from testing should be used to revise, process, and strengthen communication and reporting strategies.
Setting up a reporting system should be the power education and training aspect, including resolving all miscommunications or confusion among your team..
What Causes Poor Healthcare Documentation?
There are alot of factors causes poor healthcare documentation and that’s why the solution will be different depending on who you ask. For nurses and doctors, this may stop them from writing down the required needs of the patient or treatment, thus leading to poor documentation.
- Inaccurate Entries
- Spelling Mistakes
- Missing Information
- Copying and Pasting
- Trust drops when false information takes too long to fix
- Unidentified entries and unclear timestamps raise security concerns
By utilizing incompetent providers who don’t grasp medical terms there will be many discrepancies.
What Is Documentation Review In Healthcare?
In healthcare, documentation review checks medical records to ensure they are correctly recorded, complete, and meet certain standards. This review is critical because there are two important key points:
Quality of Care
Comprehensive and accurate medical records are necessary for quality patient care. They help doctors and other healthcare providers to follow a patient’s medical history, diagnoses, treatments, and progress. This ensures that decisions are made based on informed future care.
Reimbursement:
Documentation is required for insurance companies to pay healthcare providers. The reviewers evaluate the documentation to verify that the services provided were clinically necessary and medically warranted.
Here’s a breakdown of some key aspects of documentation review:
Who Performs It:
Internal personnel such as nurses, coders, or external experts can conduct documentation reviews, depending on the context.
What’s Reviewed:
Reviewers typically look at clinical notes, progress reports, H&P (History and physical), and other relevant information in a patient’s medical record.
What they Look For:
Other important factors are completeness, accordance, and reliability. The reviewers make sure that the documentation backs up the selected diagnoses and procedures that have been carried out.
Leveraging Technology for Smarter Healthcare Documentation
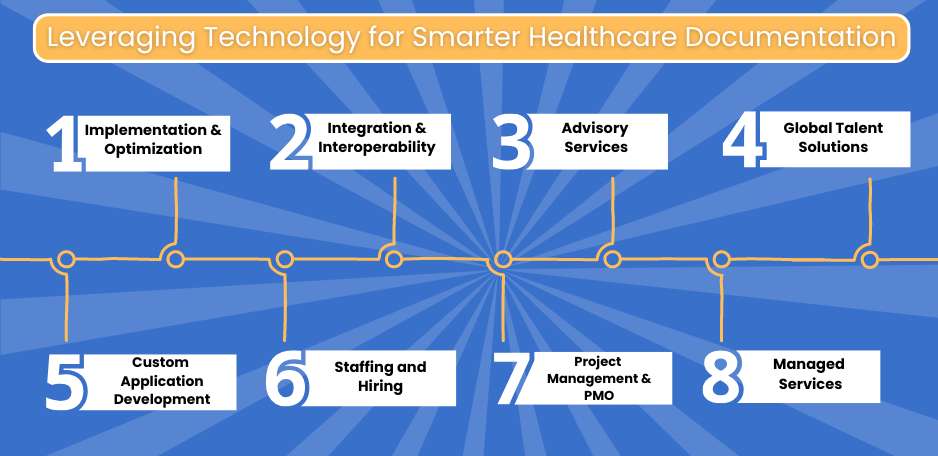
The modern digital era allows using the most up-to-date and game-changing technologies in medical documents. But Still! Is managing patient records across multiple systems causing headaches for your healthcare facility?
You’re not alone. Traditional Electronic Health Records (EHR) and Enterprise Resource Planning (ERP) systems struggle to handle medical documents’ growing volume and complexity.
Imagine a world where all your documents, patient charts, billing records, and administrative files reside in one secure, central location. Virtelligence’s bespoke software development services can create that reality. Virtelligence integrates a powerful Document Management System (DMS) with your existing EHR and ERP, giving you a unified platform to:
- Effortlessly access and manage all your documents in one place.
- Boost efficiency with features like intelligent auto-sorting and voice recognition.
- Reduce errors and improve patient care with a centralized view of medical records.
Stop wasting time toggling between systems. Virtelligence empowers you to focus on what matters most—your patients. Get the best advice today and start your hassle-free documentation journey.
Now let’s have a look at 2024’s best three technologies for smarter healthcare documentation and its improvement;
I. AI-assisted Documentation for Precision and Speed
Today’s healthcare setting has experienced a shift towards using Artificial intelligence (AI) as a tool to change the documentation process. AI is not confined to data entry; it also offers accuracy and speed in documenting patient encounters. By examining clinical notes, AI can choose the relevant ICD codes and procedures properly, thereby reducing processing time and increasing payment accuracy.
AI also helps clinical decision-making by identifying crucial information buried in huge data sets. AI is revolutionizing the healthcare industry because it streamlines document retrieval and organization with effective indexing, aiding in the availability of the whole library collection.
II. Cloud Faxing
Cloud faxing adds to Document Management Systems, making the classic fax machines disappear. Health organizations can wave bye to piles of cluttered machinery while in this new age of technology, they can opt for simplified technology that makes document exchange easy.
III. DMS With Modern Scanner Compatibility
The efficiency of document management is highly dependent on the integration of scanners. It guarantees effortless connectivity with all modern scanners, leading to the swift and easy digitization of documents. On top of that, the combination of DMS with a modern scanner saves you from compatibility problems and all the hassle of reconfigurations.
What is Clinical Documentation Improvement?
The CDI or Clinical Documentation Improvement assists clinicians in documenting a perfect EHR. All the other healthcare team members will have instant access to recent information on a given patient. Conversely, CDI (Clinical Documentation Improvement) also has many advantages.
CDI is one of the novel sections in the healthcare management sector, mainly focusing on accurate record keeping, particularly electronic health and medical records.
Compliance and Regulatory Considerations in Streamlining Healthcare Documentation
Healthcare documentation is not its ultimate goal to provide the most appropriate patient care. In addition, it is a tool for showing the authority’s compliance with regulations and creating possibilities for billing operations.
The following are the chief regulatory and compliance factors:
HIPAA Compliance:
The Health Insurance Portability and Accountability Act (HIPAA) sets specific standards for protecting patients’ private information. A healthcare document management system will inevitably be created according to HIPAA regulations to protect patient data from unauthorized access and disclosure.
Data Encryption:
Healthcare document management systems (DMS) should use encryption to store data transferred on the internet and for data storage (at rest) to stay safe. Encryption enables restrictions on unauthorized access to patient records, confirming HIPAA’s privacy standards and data integrity.
Access Controls:
Establish strict access controls and define only some of those employees who can view, edit, or delete the patient records. Role-based access control (RBAC) ensures that only authorized members can handle sensitive information.
Audit trails:
Maintain consistent audit trails to trace all activities done by any user who has accessed the patient records, modified, or shared the records. Record trails make it possible to trace whose actions triggered the problems and remain responsible, alongside regulatory compliance.
Interoperability standards:
Healthcare Document Management System, per interoperability standards like HL7 and FHIR, will facilitate efficient patient data exchange from different systems without compromising its integrity and security.
Document Authentication and Integrity:
Enforce a system to check the genuineness and the integrity of electronic documentation using digital signatures and hash functions that are effective ways to stop tampering and to ensure that the requirements of regulatory bodies for document authenticity are fulfilled.
Training and Awareness:
Regularly train your employees in regulations, compliance, and best practices for properly handling sensitive patient data. Knowledge-based programs reduce the chance of straying into non-compliance and develop a culture of compliance within the organization.
The degree of detail and difficulty of billing, coding, and clinical documentation illustrates that the road to efficiency is sustainable, leading to improved patient care. By implementing technology with process optimization, promoting collaborations, and keeping the focus on people outcomes, healthcare organizations can achieve new heights in documentation.
Recommendations To Improve Healthcare Documentation
We understand that having to do accurate healthcare documentation seems like a burden to us. Maintenance of timely and complete records can be surprisingly simple and uncomplicated.
- Note that the record reviewer is not necessarily as knowledgeable about the details as the person who wrote the entry.
- The basic requirement for high-quality EHR is to record the health status and condition of the patient meticulously.
- Make sure all other providers are also aware of the patient’s limitations.
- Validate whether the EHR tells an objective story for the patient.
- Narrate the reasons and means through which a patient’s situation is modified.
- Is all the data easily decipherable and tagged correctly?
- Every instruction will involve patients and their families.
- Care notes should outline the level of care the patient can receive.
More than 70% of survey respondents highlight that the new EHR systems should be easier to use than the ones they are already working on.
Final Thoughts
Accurate medical records are essential for patient care, billing, and legal purposes. The paper presents as inefficient; however, electronic health records (EHRs) led to better productivity but with new issues. The adoption of EHR requires the development of an easy-to-use interface, clear communication, and proper training so that mistakes can be avoided.
AI in the cloud faxing automation of documentation increases effectiveness and accuracy. However, confidentiality and privacy are paramount for HIPAA compliance data. Optimization and collaboration with the help of medical technology help healthcare organizations achieve better documentation, resulting in improved patient care.
FAQs
What is documentation in healthcare?
Documentation in healthcare is like writing a detailed report about a patient’s medical journey. It includes information about their health problems, treatments, and progress.
Why is documentation important in healthcare?
Good documentation is crucial for many reasons. It helps doctors and nurses understand a patient’s history and provide the best care. It also helps with billing and insurance purposes.
What is one of the purposes of medical documentation?
Medical documentation aims to communicate a patient’s condition and care plan to other healthcare professionals involved. This ensures everyone is on the same page about the patient’s health.
Which principle should guide the nurse’s documentation of the client’s medical record entries?
Accuracy is the most important principle for nurses documenting medical records. They should write clearly and factually about what happened to the patient during their care.
How do we reduce medical errors in documentation?
There are ways to make healthcare documentation less error-prone. Using clear and concise language, double-checking entries, and having standardized formats for recording information can all help.
Why are accurate medical coding, billing, and documentation important?
Accurate medical coding, billing, and documentation go hand in hand. Clear records ensure proper billing for services provided and help get patients the insurance coverage they deserve.
What is a healthcare documentation specialist?
A healthcare documentation specialist helps ensure medical records are accurate and complete. They may transcribe recordings from doctors or edit documents for clarity.